I. Introduction
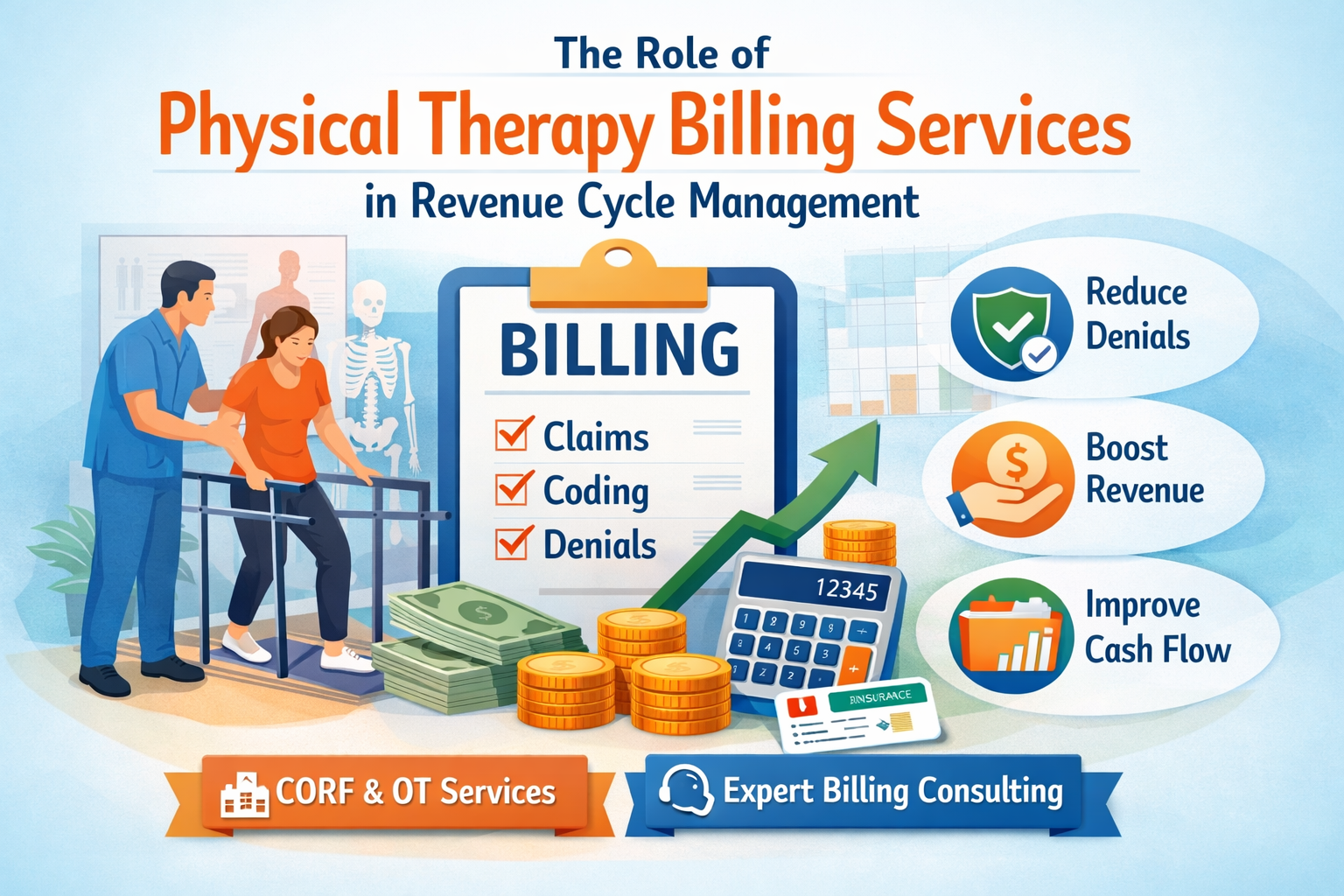
If you’ve ever worked in a therapy clinic, you already know how frustrating claim denials can be. You do everything right clinically, yet payment gets delayed or worse, denied because of a billing issue. In many cases, the problem comes down to OT Billing Units and how they are calculated, documented, and reported.
When billing units are wrong, the impact spreads quickly. Claims get denied. Payments slow down. Your staff spends hours fixing avoidable errors. On top of that, compliance risks increase, and audits become more stressful than they need to be.
The good news? Most of these mistakes are preventable. With the right understanding and habits, you can submit cleaner claims and protect your revenue cycle. In this article, we’ll walk through the most common unit-related errors, explain them in plain language, and share practical tips you can actually use in daily practice.
Think of this as a friendly conversation with someone who’s been through the same struggles and learned a few lessons the hard way.
II. Understanding OT Billing Units: The Basics
Before we talk about mistakes, let’s make sure we’re on the same page.
What Are Occupational Therapy Billing Units?
Billing units are how payers measure the amount of therapy provided during a session. Instead of billing by the visit alone, most OT services are billed based on time. That’s where units come in. Each unit represents a specific block of treatment time.
This system plays a central role in Occupational Therapy Billing, so getting it right from the start matters more than many people realize.
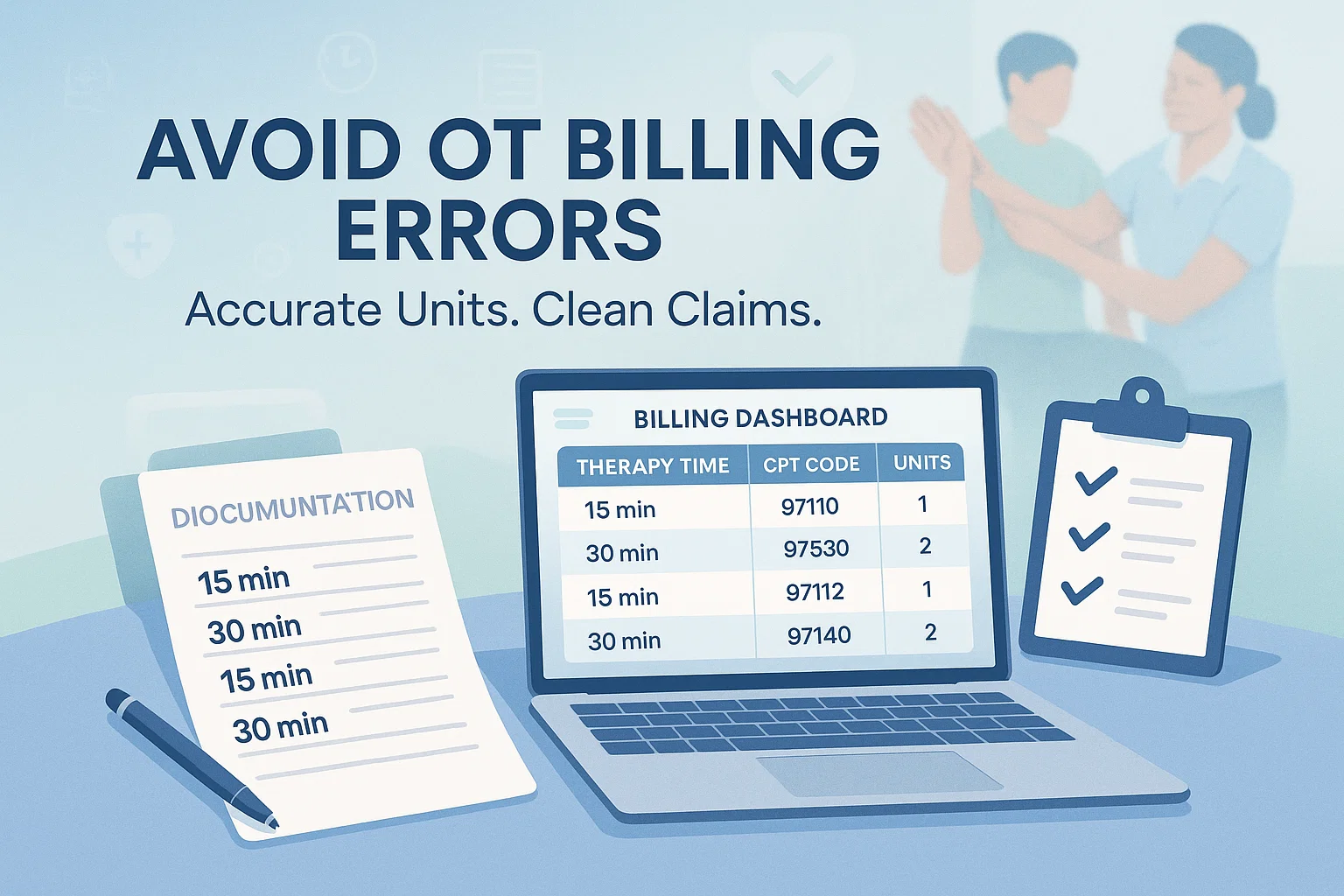
Timed vs. Untimed CPT Codes
OT services generally fall into two groups:
Timed CPT codes
These are billed based on time spent providing a service. Most timed codes follow a 15-minute structure.
Untimed CPT Codes
These are billed once per session, no matter how much time you spend. Evaluations are the most common example.
Mixing these up is one of the fastest ways to trigger denials.
The 8-Minute Rule vs. Substantial Portion Method
For Medicare and many other payers, the 8-Minute Rule applies. In simple terms:
- 8–22 minutes = 1 unit
- 23–37 minutes = 2 units
- 38–52 minutes = 3 units
Some non-Medicare payers use the Substantial Portion Method, which allows you to bill a unit when more than half of the unit time is completed.
Understanding which rule applies and when is essential. If you want a deeper breakdown, resources like The Ultimate Guide to OT Billing Units can help clarify these rules in a simple way.
Common OT CPT Code Categories
Most OT services fall into categories such as:
- Therapeutic activities
- Therapeutic exercises
- Neuromuscular reeducation
- Self-care and home management training
Each category has its own billing rules, and confusion between them often leads to errors.
III. Common OT Billing Unit Mistakes That Lead to Denials
Let’s talk about where things usually go wrong.
1. Misapplying the 8-Minute Rule
This is probably the most common issue.
Some clinics bill one unit even when the service lasted only five or six minutes. Others bill multiple units for short sessions that don’t meet the required time.
It gets even trickier when multiple timed services are provided in one visit. Combining minutes incorrectly can quickly push a claim into denial territory.
2. Mixing Timed and Untimed Codes Incorrectly
Untimed codes should be billed once per session period. Yet it’s not unusual to see them billed multiple times or added into total time calculations.
This mistake often happens when documentation templates aren’t clear or staff aren’t fully trained on code definitions.
3. Inaccurate Time Documentation
This one sounds small, but it’s a big deal.
Rounded times. Estimated times. Missing start and stop times. All of these raise red flags during claim review.
Payers want to see clear evidence of how long services were provided. Without it, even valid care can go unpaid.
4. Duplicate or Overlapping Services
This issue often shows up when OT and PT services happen on the same day. Without clear documentation, payers may see the services as overlapping.
Clinics that also offer Physical Therapy Billing Services or Respiratory Therapy Billing Services need to be especially careful here. Each discipline must show distinct, skilled care to avoid denials.
5. Using Incorrect CPT Codes
Outdated codes, wrong evaluation codes, or mismatches between notes and billed services can all cause problems.
It’s not always about intent. Sometimes, it’s just a matter of not keeping up with annual code updates.
IV. Documentation Errors That Trigger Claim Rejections
Even when units are calculated correctly, poor documentation can sink a claim.
Payers expect to see:
- Clear justification for skilled OT services
- Functional goals tied to treatment
- Complete daily notes and progress reports
- A strong link between services and measurable outcomes
This is where The Role of OT Billing Units in Occupational Therapy Billing becomes clear. Units don’t stand alone. They must be supported by solid, consistent documentation.
V. Payer-Specific Billing Unit Challenges
Not all payers play by the same rules, and assuming they do is risky.
Medicare
Medicare is strict about the 8-Minute Rule and documentation standards. Small errors can quickly lead to denials or audits.
Medicaid
Rules vary by state, which adds another layer of complexity.
Commercial Insurance
Some commercial payers follow Medicare rules, while others don’t. This inconsistency catches many clinics off guard.
Clinics offering Corf Billing Services or Respiratory Therapy Billing Services often face additional payer-specific rules, making it even more important to review payer manuals and LCDs regularly.
VI. Best Practices for Accurate OT Billing Units
Now let’s talk solutions.
1. Standardize Time Tracking
Use clear start and stop times for every service. Avoid estimates. EMR templates can help enforce consistency across providers.
2. Match Documentation to Billed Units
Every billed unit should be easy to justify by reading the note. If a reviewer can’t connect the dots, you’re at risk.
3. Conduct Regular Internal Audits
Audits don’t have to be scary. Simple internal reviews can catch patterns of errors before payers do.
4. Educate Therapists and Billing Staff
Billing accuracy improves when therapists and billers work as a team. Regular training helps everyone stay current and aligned.
VII. Tools and Checklists to Prevent OT Billing Errors
Sometimes, the simplest tools make the biggest difference.
A daily billing checklist can help staff confirm:
- Total treatment time
- Correct unit calculation
- Proper code selection
Quick-reference guides like The Ultimate Guide to OT Billing Units are especially helpful for busy clinics that also manage Physical Therapy Billing Services alongside OT.
EMR alerts and routine updates to CPT and CMS guidelines also reduce avoidable errors.
VIII. Real-World Examples of OT Billing Unit Errors
Example 1: The 8-Minute Rule Misstep
A therapist provided 18 minutes of therapeutic exercise and billed two units. The claim was denied. Why? The time didn’t support it.
Example 2: Weak Documentation
Units were correct, but notes didn’t explain why the service was skilled. The payer denied the claim.
Example 3: Overlapping Services
OT and Corf Billing Services were billed on the same day without clear differentiation. The payer flagged it as duplicate care.
Each case shows how small issues can have big consequences.
IX. Compliance and Audit Readiness
Billing unit errors don’t just affect payment. They increase audit risk.
Strong documentation, consistent processes, and staff education all support compliance. This is another place where The Role of OT Billing Units in Occupational Therapy Billing comes into focus. Units, notes, and compliance are deeply connected.
X. Conclusion
Most billing problems aren’t caused by bad care. They’re caused by small mistakes that add up over time.
By focusing on accuracy, training, and clear documentation, clinics can avoid common errors with OT Billing Units and improve claims approval rates. Strong billing practices also support better cash flow and reduce regulatory stress.
At the end of the day, clean claims support better care. And that’s something we can all get behind in Occupational Therapy Billing.
XI. Frequently Asked Questions
How many OT units can be billed per session?
It depends on total treatment time and payer rules.
Can OT and PT units be billed on the same day?
Yes, but documentation must clearly show distinct services.
What is the most common OT billing error?
Misapplying the 8-Minute Rule.
How often do CPT rules change for OT billing?
Updates typically happen annually, but payer policies can change more often.