Let’s suppose you are a medical billing specialist in a respiratory care center. You must be managing revenue cycle management (RCM) workflow that includes creating accurate documentation, coding, and billing for pulmonary rehabilitation and diagnostics. While performing pulmonary therapy billing practices, you must have observed billing challenges such as missing modifiers, incorrect PFT coding, time-based billing errors, and missing signatures. Insufficient documentation of medical requirements causes denial in payment procedures. Moreover, the transition from old codes to new ones creates confusion and makes the billing framework more complicated. Continuous loopholes in billing also reduce the average Days Sales Outstanding (DSO) to 55 days and result in excessive revenue loss.
To optimize pulmonary billing workflows, the respiratory health centers have transformed their manual processes to specialized, technology-driven revenue cycle management (RCM) approaches. Before treatment, the billing officer conducts patient documentation by employing the Electronic Health Records system. It involves automating documentation such as generating comprehensive records of a patient’s personal data, medical history, lab results, X-rays, and other clinical findings. Moreover, the tools check the insurance eligibility of patients and also perform prior authorization for high-cost procedures such as bronchoscopy and CPAP setups in case of complexity.
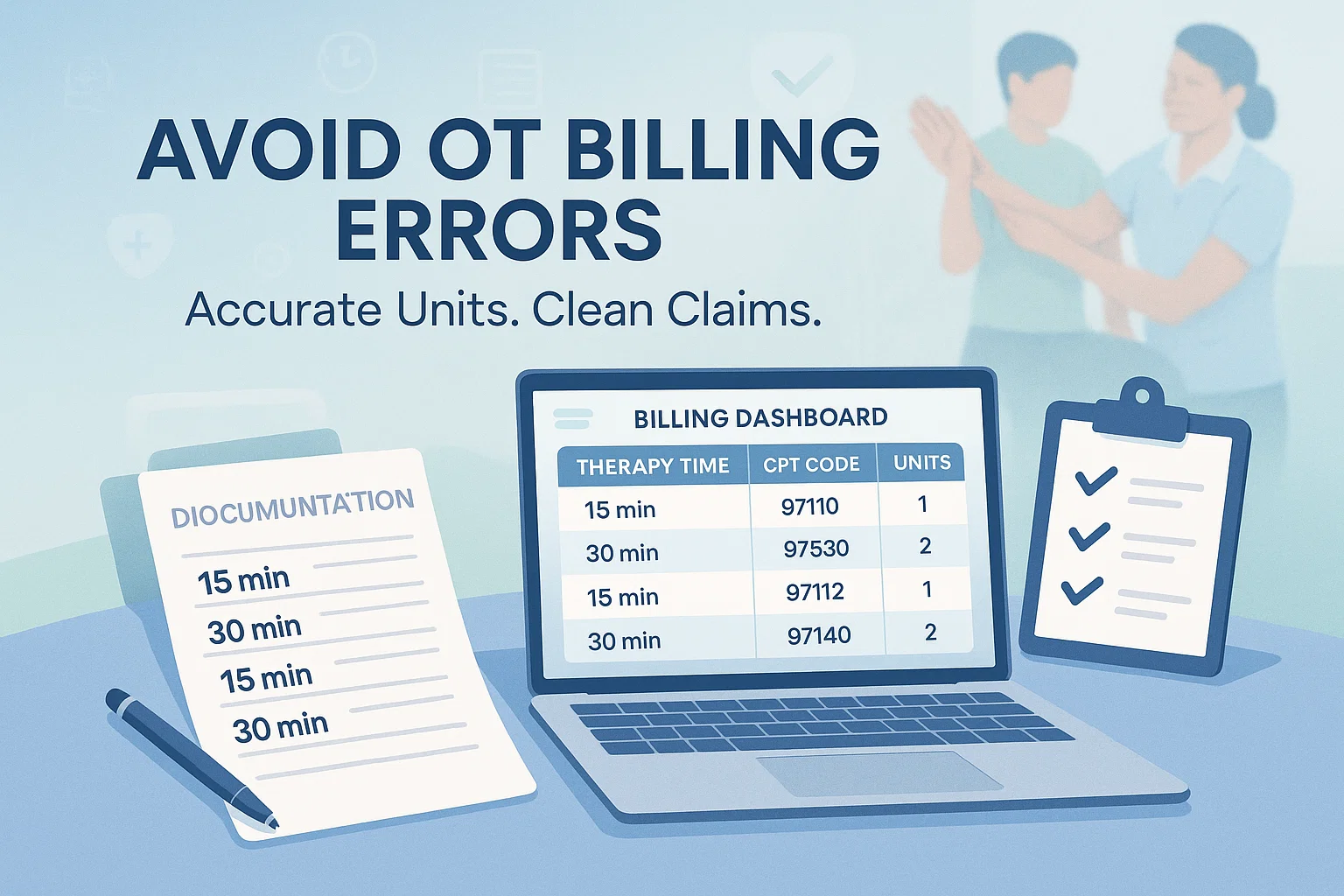
AI-Powered RCM converts therapy sessions into standardized codes, such as CPT for services and ICD-10 for diagnoses. Employing durable medical equipment, perform real-time verification of patient insurance coverage, such as checking patient insurance eligibility, and track the status of payment from submission to reimbursement.
A comprehensive guide to billing allows therapists, billing teams, and medical practitioners know the significance of streamlining billing procedures for revenue cycle efficiency. AI – driven tools provide strategic and operational assistance to respiratory care services. The billing department employs automated tools, such as AI-powered Robotic Process Automation (RPA), Intelligent Document Processing (IDP), and Electronic Health Record (EHR), to reduce administrative burdens and minimize coding errors. The tools streamline billing practices such as accurately documenting patient information, automatically scanning clinical documentation, such as clinicians’ notes, identifies and coding billable services. Employing these technology-driven tools has helped pulmonology services to conduct regular audits to maintain compliance standards, ensure full reimbursement to patients, and accelerate their revenue cycles.
Understanding Pulmonary Therapy Billing Basics
What Pulmonary Therapy Billing Covers
Pulmonary Rehabilitation
Pulmonary Rehabilitation billing includes a comprehensive program that includes therapeutic exercises. Physical exercise and training comprise endurance-building workouts, body mechanics, conditioning, and movement therapy exercises. Breathing exercises improve respiratory function, such as diaphragmatic breathing and pursed-lip breathing, and help relax the body. Pulmonary rehab covers education for respiratory patients. It includes patient-tailored pulmonary rehabilitation programs that provide self-management training to help patients manage their lung condition and perform daily activities with less breathlessness.
Pulmonary therapy billing also encompasses an occupational respiratory therapy program comprising breathing training, muscle strengthening/endurance, breathing retraining exercises, pursed-lip breathing, energy conservation, and airway clearance techniques. Lifestyle education provides nutrition counseling and smoking cessation. Ventilation assessments involve distinctive coded procedures to monitor and treat a patient’s ability to breathe and exchange gases. These services are generally covered by Medicare and private insurers by using specific CPT codes used for diagnostic, management, and therapeutic services.
Key Coding Systems Used
The therapists use different HCPCS codes for pulmonary rehab services. For instance, CPT code G0424 is used for pulmonary rehabilitation, per session, which includes exercise, education, and psychosocial assessment. For outpatient PR, MD/HCP services, per session, the therapists use CPT 94625. The code, G0237, is used for therapeutic procedures and to improve pulmonary function. Other relevant CPT codes, such as 97110, are used for neuromuscular re-education and self-management techniques.
ICD-10 Diagnosis Codes Support Medical Necessity
ICD-10 codes support medical necessity by linking specific patient diagnoses to procedures. Specific ICD codes, such as E11.9 is used for chronic Type 2 Diabetes, to cure UTI, practitioners use N39.0, and the code used for fatigue is R53.83.The other detailed codes, such as E78.2 is used for Mixed Hyperlipidemia and E55.9 for vitamin D deficiency.
HCPCS Codes where Applicable
HCPCS (Healthcare Common Procedure Coding System) codes are used for billing supplies, equipment, medications, and non-physician services. They are divided into HCPCS Level I and Level II. HCPCS Level I includes CPT Codes for physician services, procedures, and outpatient services. HCPCS Level II Code classifications include codes for medical transportation, such as ambulance services, hospital outpatient settings, and dental procedures. People use HCPCS codes to access medical equipment such as wheelchairs, oxygen, and hospital beds. For medical, surgical, Orthotics/Prosthetics services, the patient’s family uses Land M codes, while P codes are used for obtaining specimen collection from the laboratory.
Payer Categories
Medicare
Medicare Part B includes outpatient pulmonary rehabilitation up to 36 sessions, or adding 3 more sessions. Medicare Part A: Covers inpatient services such as hospitalization, requiring expert nursing facilities, and nursing home facilities.
Medicaid
Includes medical coverage guidelines for patients with chronic respiratory diseases. Medical policy varies significantly by state, as different nation states manage their own Medicaid programs, setting and unique insurance regulations.
Commercial Insurance
Commercial health insurance includes a comprehensive coverage plan for private insurers. An employer-sponsored plan offered by companies, such as PPO, HMO, EPO, and POS, covers the diagnosis and treatment of chronic pulmonary diseases.
Workers Compensation
Workers’ compensation insurance is a compulsory employer-paid insurance that covers medical rehabilitation for employees injured or developed potential disabilities due to a harsh and unsafe job environment. Medical expenses are provided in the form of partial income replacement for time missed due to injury. Health insurance covers doctor visits, hospitalization, prescriptions, physical/occupational therapy, and vocational training for new careers. Additionally, workers’ compensation insurance also offers death benefits encompassing funeral costs and providing financial support for dependent family members.
Common Barriers to Fast Pulmonary Therapy Payments
Incomplete or Incorrect Documentation
Partial documentation in pulmonary therapy billing causes claim denials and lost revenue. It includes missing treatment notes, such as incomplete patient responses to treatment, progress notes, and session duration. Patient records lack a physician or non-physician practitioner (NPP) signature on the Plan of Care (POC). Improper documentation also includes mismanagement in using modifiers to access separate therapy services. Failure to document timed services causes issues with the 8-minute rule.
Coding Errors
Loopholes in pulmonary therapy billing involve improper coding. Both payers and therapists should know about updated billing codes. Many recipients either use outdated or incorrect CPT code selection that leads to instant denials. Sometimes the billing team fails to pair HCPCS codes with the precise ICD-10 diagnosis code for effective diagnosis and treatment. The wrong calculation of time-based codes and using multiple therapy codes create a lack of focus in the treatment plan. Misplaced or dangling modifier causes rejections and financial penalties.
Delayed Claim Submission
Complexity and strict documentation requirements in pulmonary rehabilitation allow payers to set strict deadlines for submission of insurance claims. Insurance claim filing timeframes vary, as general policy limits include 90 days to 12 months for submitting complete documentation. Some insurance companies allow people to initiate a request for compensation within 72 hours to 30 days. Delays in submitting claims cause non-acceptance of claims and lead to huge loss of reimbursement.
Workflow Inefficiencies
Another challenge that billing specialists encounter is the documentation burden. They rely on manual data entry that causes documentation gaps and errors. Comprehensive coding procedures require detailed notes, physician signatures, a complete session time log, correct code selection, accurate time-based code, recovery goals, and progress reports of the patient. If any one of these details is missed from documentation, it causes instant rejection or delay in reimbursement.
Insurance Verification Issues
Therapists fail to verify the insurance eligibility of the patient due to improper documentation. It includes data entry errors such as misspelled names, incorrect date of birth, wrong registration number of the patient, outdated CPT codes, and inaccurate insurance information makes it difficult for billing specialists to verify insurance eligibility.
Step-by-Step Strategies to Streamline Pulmonary Therapy Billing
Implement Strong Front-end Processes to Verify Insurance Eligibility
The pulmonary rehab requires insurance companies, such as Medicare, to perform prior authorization of the patient’s insurance eligibility and determine if prior authorization is required for complex procedures such as bronchoscopy or PAP device setup. The authorization details should include the number of sessions for the patient. The standard Medicare insurance plan covers up to 36 sessions, extended to 72 sessions in special cases. The therapist should meticulously check the number of therapy sessions required and the medical necessity requirements before the session. Gather accurate patient demographics and record all authorization details in the EHR system to ensure billing compliance.
Standardize Documentation Procedures
Clinical documentation conducted by medical billing services includes procedure details, medical necessity, documenting the procedural time, and maintaining daily, accurate session notes. Healthcare providers gather personal and financial information from a patient at the time of appointment to verify insurance coverage and ensure accurate billing. They create templates for pulmonary therapy notes and maintain up-to-date patient documentation.
Improve Coding Accuracy
Once clinical documentation is done, medical coders analyze physician notes, lab results, and treatment plans. The updated CPT, ICD-10, and HCPCS guidelines help coders to translate physician notes, diagnoses, and procedures into standardized codes such as ICD-10 and CPT for insurance claims. The coders conduct regular coding audits, cross-check, and verify medical codes to ensure accuracy, compliance, and proper reimbursement.
Automate Claim Submission & Tracking
Medical billing companies submit claims using electronic billing software or through payer portals. They automate necessary supporting documentation such as pulmonary function tests, cardiology reports, discharge summaries, and breath management exercises. Employing billing software helps track claim status in real-time and sends alerts for pending or rejected claims.
Strengthen Communication between Therapists & Billing Teams
To reduce claim denials, automate cash flow, and enhance overall pulmonary therapy billing practice requires therapists and the billing department to coordinate and conduct regular audits and weekly documentation reviews. For quick collaboration, the teams use an integrated messaging system to discuss specific billing issues and obtain updated patient information, treatment plans, and progress notes. Establishing standardized communication protocols help billing department to set deadlines for documentation completion, signing evaluations, and progress notes within 24–48 hours. Centralized record management helps therapists and the billing department to work together to find missing patient information, updated patient insurance coverage, new CPT codes, and fulfill other documentation requirements.
Monitor Insurance Requirements Regularly
The final process involves billing teams tracking the revenue cycle. Regular audits reveal the causes for claim denials, such as missing prior authorizations, non-covered supplies like PAP devices, and inaccurate time-based coding for pulmonary rehabilitation. Moreover, monitoring KPIs such as denial and clean claim rates shows loss of revenue due to operational inefficiency. The evaluation, comprising quarterly training and policy updates keep staff aligned with CMS rules. The therapists and billing teams leverage technology to automate billing workflow, spot recurring coding and documentation errors, and improve their efficiency.
Regular monitoring of insurance requirements in pulmonary billing organizes and continuously updates a centralized, digital library of all health insurance coverage, medical policies, and administrative rules from various insurers. The billing staff remains updated with new regulatory requirements for pulmonary rehab (PR) and diagnostic tests, and keeps up-to-date with new Medicare pulmonary rehab rules, PFT and diagnostic coding, and rehabilitation codes.
Best Practices for Faster Reimbursement
Reduce Denials with Proactive Checks
To achieve faster reimbursement in pulmonary billing, the patient is required to verify insurance coverage 24–48 hours before the scheduled appointment. Perform prior authorization and confirm medical necessity criteria, such as the requirement of advanced technology and resources, such as Bronchoscopies, Lung Biopsies, and certain DME (Oxygen/CPAP) to treat chronic lung diseases. The therapist uses automated tools to track PA numbers and ensure they are linked to the claim before submission. Accurate and verified patient documentation, active coverage, prior authorization, and coordination with therapists before services prevent claim rejection. With double-check documentation before submission, the billing team verifies the patient’s name, date of therapy services, case numbers, and contact information. Moreover, they ensure that the signatures of the therapist and other supporting documentation is enlisted to prevent any mishap in the billing procedure.
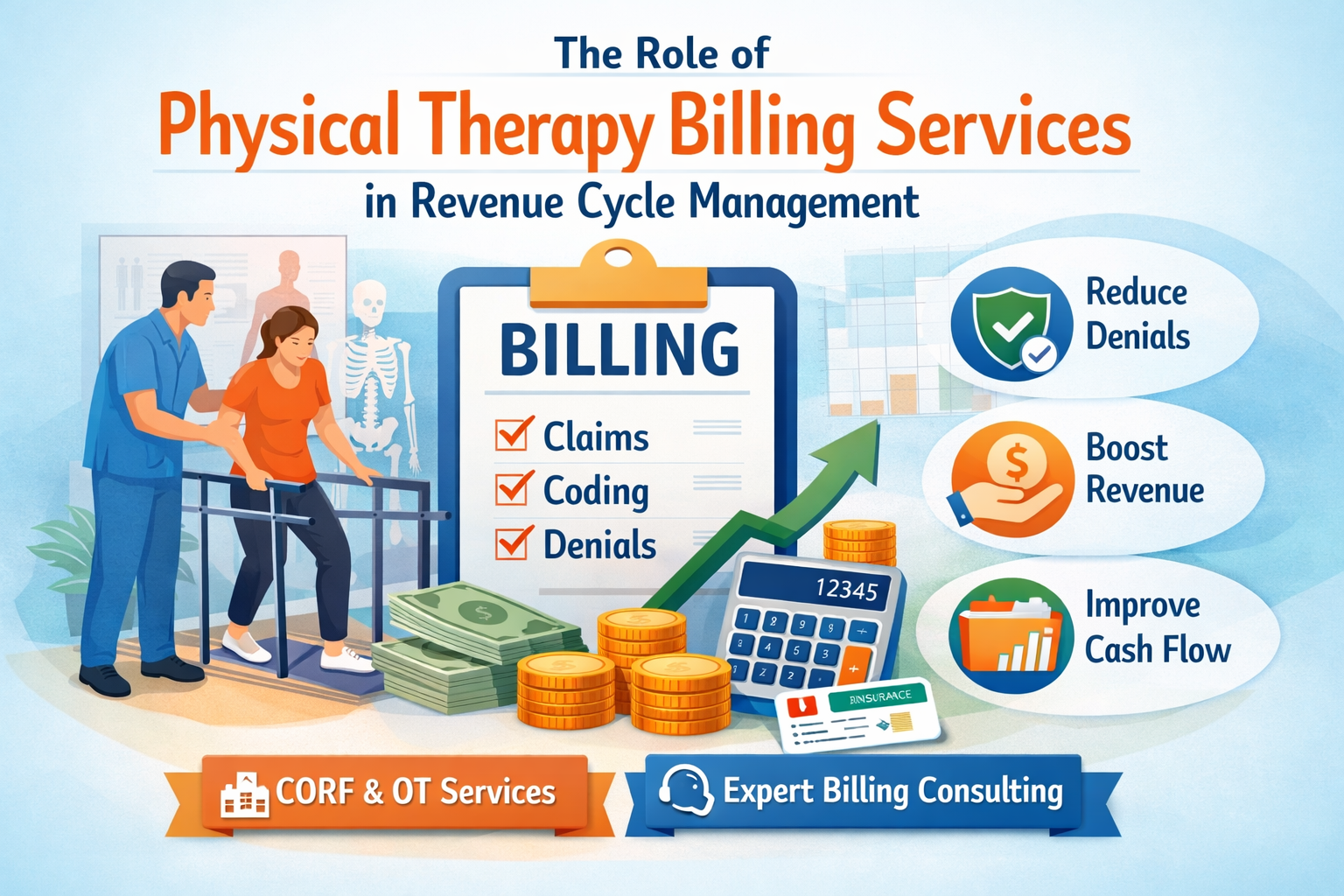
Optimize Revenue Cycle Management (RCM)
The billing department in respiratory care centers increasingly uses automated tools such as automated Revenue Cycle Management to streamline financial processes from patient registration to final payment collection. The automated system adjusts workflow based on data insights, detecting errors in patients’ documentation such as missing information and incorrect codes. The dashboards and analytics help in eligibility verification, such as instantly checking patient insurance coverage, verifying confirmed insurance, deductibles, and co-pays at the point of scheduling or registration to avoid denials. The Robotic Process Automation feature in RCM ensures fast and smooth online payment options to speed up patient collections. The automated tool further assists the billing department in maintaining accuracy and compliance in billing and accelerates the revenue cycle.
Specific EHR & Practice Management
An EHR (Electronic Health Record) Practice Management is an integrated software combining clinical data management with administrative/financial tasks. The billing department integrates EHR in its billing system to manage patient documentation comprising medical history, diagnoses, medications, lab results, and treatment plans. Moreover, the therapists handle patient registration, coding, and conduct real-time eligibility verification. The integrated systems improve patient care, ensuring quicker access to records, prompt communication, and streamlined payment processes.
Targeted Automation & Coding Tools
MediCodio, an AI-powered tool, uses machine learning and NLP to analyze pulmonary clinical documentation, read a therapist’s narrative notes, and translate them into the correct ICD-10 and CPT codes to reduce manual workload. Therapists use CodaMetrix to interpret provider notes and assign codes across various pulmonary procedures. The tool, MaxRemind, offers specialized pulmonary rehab billing services such as tracking denials in real-time. It minimizes denials and ensures quick reimbursement.
Telehealth Integration & Its Billing Impact
The medical billing department has been transformed through Telehealth services. The coding system, insurance claims, and patient billing have been modified. Telehealth has automated and streamlined billing processes by eliminating errors in documentation and coding. Consequently, assist the billing department in enhancing its billing operations. Telehealth provides specific modifiers such as -95, -93, -GQ that indicate that the pulmonary therapy service is virtually provided to the patient. Employing Telehealth helps patients with more efficient and faster consultations, reducing the overhead cost of travelling to a physical health center. To know telehealth regulations, including licensure requirements and reimbursement policies, patients can navigate different state regulations and international policies to learn about the evolving regulations of telehealth billing services.
Compliance Considerations
Respiratory care billing compliance requires pulmonary health centres to maintain strict adherence to documentation standards, medical necessity rules, and coding accuracy. To meet HIPAA standards, pulmonary practices ensure that patient records, claims data, and images must be encrypted during transmission through emails or stored in Electronic Health Record (EHR) systems. Respiratory centres conduct regular HIPAA training for the staff to maintain secure documentation. They ensure safe transmission of patient data, preventing unauthorized access to view or modify patient data.
Implementing specific compliance requires pulmonary rehabilitation clinics to develop a pulmonary rehabilitation plan that will be reviewed every 30 days by the internal controls team. They use AI-driven, HIPAA-compliant coding tools to identify errors such as incorrect patient information, missing time logs, and improper code selection and physician notes to prevent claim rejection.
Medicare Pulmonary Rehab Guidelines
The Medicare guidelines for pulmonary rehabilitation continue to prioritize chronic obstructive pulmonary disease (COPD) patients. Medicare Part B provides pulmonary rehab for patients with moderate to very severe COPD, interstitial lung disease (ILD), bronchiectasis, pulmonary fibrosis, and cystic fibrosis based on the diagnostic report.
Session limits and duration prescribed by Medicare include 36 sessions to be delivered 2–3 times per week. The session includes therapy exercises such as aerobic exercise, which is mandatory in each session. The therapy session lasts at least 31 minutes or 91 minutes for two sessions. The specific respiratory equipment used in therapy session include airway clearance and lung expansion devices, equipment to improve lung function, deep breathing, and examine lung volume. Mechanical ventilators are used for patients with acute care, needing breathing support.
Extended coverage includes telehealth flexibility. It includes education/counseling provided via telehealth. Remote Patient Monitoring (RPM) codes are billed with pulmonary rehab billing services.
Recap
New respiratory billing therapists find the billing process highly time-consuming and complex. Outdated payment structures, manual data entry, insurance verification, prior authorization, and strict documentation requirement makes pulmonary rehabilitation billing challenging for therapists and billing teams. An inexperienced therapist fails to understand complex coding and documentation that leads to under-billing. Improper time-based documentation, code selection, outdated coding, and inadequate information on patients’ insurance coverage cause rejection or delay in compensation. The reality is that without a streamlined billing process, the therapist and billing teams are unable to overcome operational and administrative challenges and continue to face administrative burdens.
Streamlining pulmonary therapy billing requires a focus on reducing claim denials through precise documentation, automated technology, and proactive, specialized coding. By implementing advanced technology such as AI-powered billing software automatically detect errors, such as missing modifiers or incorrect codes, before submission. The software helps in coding and documentation, and insurance verification to avoid claim denials. The therapist employs electronic Payments and funds transfer tools to speed up cash flow, eliminate manual posting, and ensure faster payments. Medical billing companies also outsource specialized billing by partnering with a dedicated pulmonology billing company to handle complex and high-volume claims to ensure accuracy and compliance. The billing department automates patient payments through patient portals and text-to-pay to collect patient payments faster. To determine pulmonary care billing compliance, respiratory care centres stay in compliance with HIPAA standards to safeguard electronic protected health information during documentation and transmission of data through email or to clearinghouses and stored in Electronic Health Record (EHR) systems. Staying adherent to Medicare guidelines for pulmonary rehab allows therapists to conduct 36 therapy sessions for patients with severe or mild COPD, post-COVID respiratory issues, and pulmonary hypertension. Compliance considerations require respiratory centres to conduct regular internal audits to review denial trends and ensure accurate coding. Comprehensive staff training covers pulmonology-specific coding and management. Training also helps therapists comprehend documentation standards required for high-risk areas like pulmonary rehab and sleep studies. The training sessions keep staff updated with Medicare/CMS rules, such as changes in telemedicine, critical care, and billing practices. To avoid fraud in coding practices and ensure accuracy in claims, billing teams use AI-driven tools to identify errors before submission. The tools ensure proper coding, optimize documentation, monitor denial rates and improve revenue cycle management.