I. Introduction
If you’ve ever worked in a healthcare billing department, you know how stressful the process can feel. One small mistake can delay payment for weeks. Sometimes even months. And when it comes to respiratory therapy billing, the process gets even more detailed. Most billing teams juggle complex codes, strict documentation rules, and changing payer policies. It’s a lot to keep up with.
Accurate billing isn’t just about avoiding confusion. It directly impacts cash flow, compliance, and the overall financial health of a practice. When claims go out with mistakes, you often deal with denied claims, delayed reimbursements, and frustrated staff. These issues add pressure to teams that are already managing heavy workloads.
That’s why understanding the most common errors—and how to prevent them—matters so much. The good news? Most mistakes are fixable. Many are actually preventable with better training, simple process improvements, and more consistent communication.
In this article, we’ll walk through the most frequent respiratory therapy billing problems, explain why they happen, and share practical strategies to solve them. By the end, you’ll feel more confident in recognizing these issues and stopping them before they interrupt your billing workflow.
II. Understanding Respiratory Therapy Billing
Before we jump into the mistakes, let’s look at what respiratory therapy billing actually involves. Many people outside the field assume it’s just “sending a claim.” But the process includes many moving parts.
A. What Respiratory Therapy Billing Includes
Respiratory therapy billing covers a wide range of services that help patients breathe and recover from lung-related conditions. Some common treatments include:
- Oxygen therapy
- Pulmonary rehabilitation sessions
- Nebulizer treatments
- Airway management
- Spirometry testing
Each service requires specific documentation. For example, oxygen therapy needs a physician order, oxygen saturation measurements, and medical necessity notes. Pulmonary rehab often requires time tracked logs and therapist signatures.
Good documentation is the foundation of accurate billing. When notes are missing, incomplete, or unclear, claims often end up denied.
B. Key Payers Involved
Respiratory therapy services are billed to different payers, such as:
- Medicare
- Medicaid
- Commercial insurance companies
- Workers compensation programs
Each payer follows its own rules. Medicare might require specific modifiers, while a commercial payer might need extra authorization. Missing just one requirement often leads to a denial.
C. Importance of Accurate CPT, HCPCS, and ICD-10 Codes
Correct coding is the backbone of billing. When codes don’t fully match the service provided, claims bounce back.
Incorrect codes often happen when:
- A code update wasn’t reviewed
- Staff members guess instead of verifying
- Documentation lacks enough detail to assign the correct code
A simple code mismatch can cost a practice thousands of dollars over time.
III. Most Common Respiratory Therapy Billing Errors
Let’s look at the issues that billing teams face most often. These errors show up across many practices, no matter their size. Many of the Respiratory Therapy Billing Errors listed below are extremely common even in well-managed clinics.
1. Incorrect or Outdated CPT/HCPCS Codes
This is one of the top reasons insurance companies deny claims. Codes change every year. If your practice doesn’t stay updated, you might bill with old or deleted codes.
Another common issue is selecting a code that doesn’t match the actual service. For example, coding a simple nebulizer treatment as a complex airway procedure. Insurance systems flag mismatched codes right away.
2. Incomplete or Missing Clinical Documentation
Missing documentation is a huge problem in many therapy practices. It happens when:
- The physician’s order is not filed correctly
- Therapist notes are incomplete
- Time logs are missing
- Medical necessity isn’t clearly explained
- Therapist signatures are missing
If documentation doesn’t prove the service happened, insurance companies will deny the claim. Every time.
3. Billing for Non-Covered or Non-Authorized Services
Sometimes the service is provided, but the payer doesn’t cover it.
This usually happens when:
- Staff forgets to check coverage
- No prior authorization was obtained
- A service is experimental or not medically necessary
It’s frustrating because the care was delivered, but the reimbursement gets denied.
4. Upcoding or Undercoding
Upcoding is when a higher-level service is billed without proper documentation. Undercoding happens when a lower-level code is used, leading to lost revenue.
Both mistakes cause problems.
Upcoding can lead to audits and penalties. Undercoding results in reduced payment for work actually performed.
5. Duplicate Billing
Duplicate billing happens more than people think. It can occur when:
- A claim is submitted twice accidentally
- Software glitches duplicate entries
- Two staff members bill the same patient on the same date
Insurance systems catch duplicates quickly. But they still slow down payment and create extra work for billing teams.
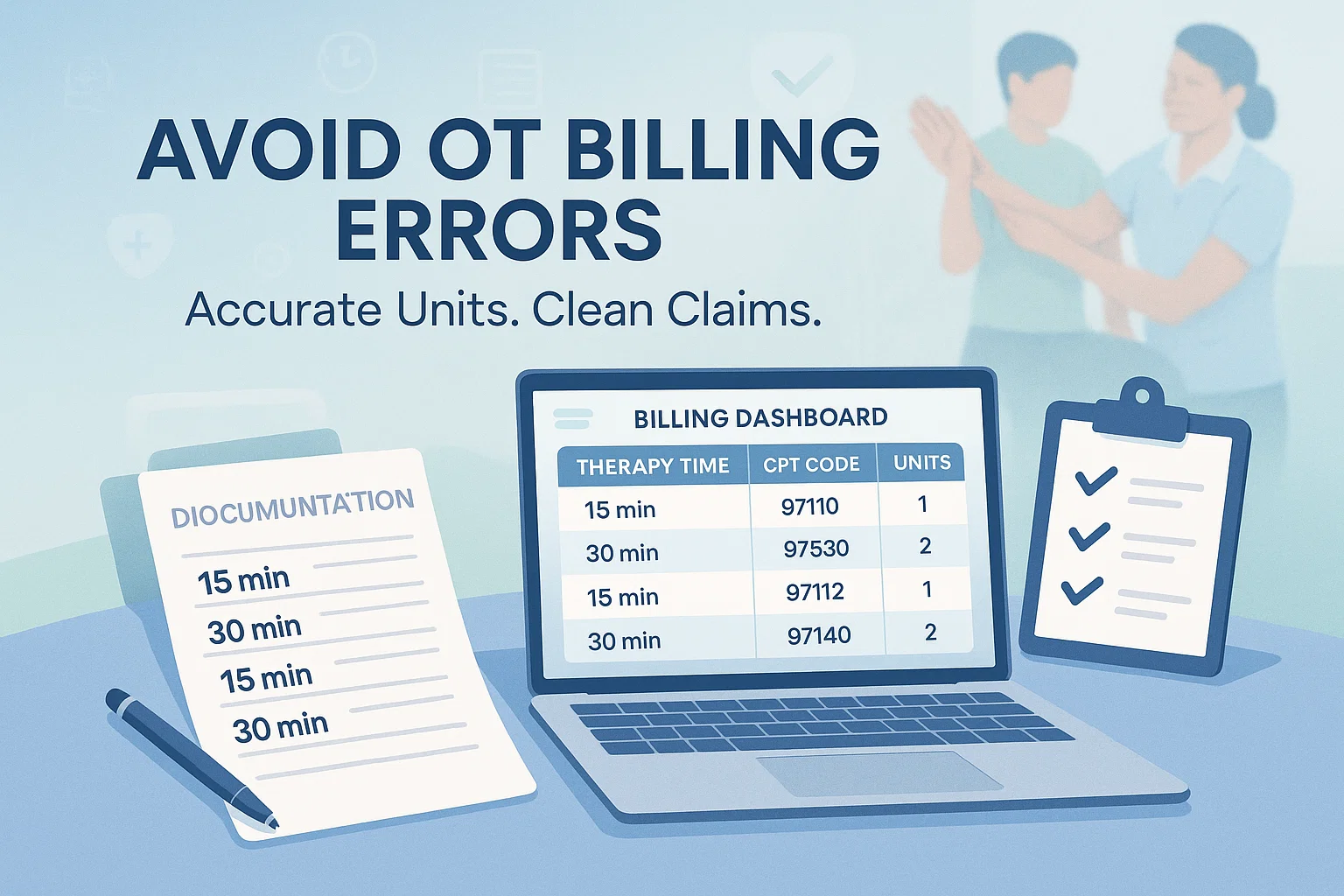
6. Incorrect Modifiers or Missing Modifiers
Modifiers show details about how and why a service was performed. If a modifier is missing or incorrect, the claim doesn’t make sense to the payer.
For example:
- Modifier 59 is used for separate procedures
- RT and LT indicate right or left side
- Modifier 76 shows a repeated service
Using the wrong modifier can lead to denials, confusion, or underpayment.
7. Incorrect Patient Information
This may sound simple, but incorrect patient details are surprisingly common. Billing teams deal with misspelled names, wrong dates of birth, incorrect policy numbers, or outdated insurance information. Even a small typo can lead to a rejection.
8. Not Updating Insurance Rules and Payer Guidelines
Insurance rules change constantly. Medicare updates happen yearly. Commercial payers revise policies often. If your staff doesn’t keep track, claims may not meet new rules.
Outdated knowledge can lead to repeated denials and long delays in payment.
9. Errors in Charge Capture
Charge capture errors occur when services are not entered into the billing system correctly.
This happens when:
- Staff forgets to record certain treatments
- Multiple sessions aren’t logged
- Manual entry leads to mistakes
These mistakes often mean lost revenue because the service wasn’t billed at all.
10. Delayed Claim Submission
Each payer has deadlines for submitting claims. If your team misses the deadline, you may lose the chance to bill altogether. Even when the claim is accepted, delays slow down reimbursement and create cash-flow issues.
IV. How These Billing Errors Impact Reimbursement
Billing mistakes don’t just create temporary frustrations they have real financial consequences.
A. Financial Consequences
Each error costs time and money. Denied claims need to be corrected and resubmitted. That takes extra labor. Delays can also stress the practice’s financial stability. Over time, these mistakes create revenue leakage money the practice earned but never collected.
B. Compliance Risks
Accuracy is essential for compliance. Upcoding, missing documentation, or inconsistent billing patterns can trigger audits. Some audits lead to penalties or repayment demands. Practices must protect themselves through careful billing and consistent checks.
C. Operational Challenges
When claims get denied, staff spend time fixing errors instead of focusing on new claims. This leads to:
- Stressful workloads
- Slower payment cycles
- Disrupted patient care workflows
It impacts the whole team, not just the billing department.
V. Best Practices to Avoid Respiratory Therapy Billing Errors
Now let’s explore how to prevent these issues. The good news is that small improvements can make a big difference.
A. Implement Regular Coding Training
Coding changes every year. Your team should receive regular training to stay updated. Even quick monthly updates can prevent costly mistakes.
B. Strengthen Documentation Processes
Clear and complete documentation can prevent many errors. Use standardized templates. Ensure therapists complete notes in real time. Verify physician orders before billing.
C. Use Respiratory Therapy Billing Software
Modern billing software can save time and prevent errors. Many systems offer:
- Automated coding suggestions
- Real-time error alerts
- Charge capture features
- Claim tracking tools
These systems also integrate with electronic health records. Features like these make the billing process easier and more accurate. Many clinics also adopt programs similar to Tools and Software to Simplify Medicare Billing, which help reduce manual errors and improve compliance.
D. Conduct Routine Internal Audits
Regular audits help identify trends in denials. Quarterly or even monthly checks can prevent recurring mistakes. They also help teams catch documentation gaps before claims go out.
E. Verify Eligibility and Authorization Upfront
Always verify insurance coverage before services begin. Real-time eligibility checks help ensure services are covered. This prevents denied claims due to authorization issues.
F. Utilize Correct Modifiers Consistently
Create easy reference sheets for modifiers. Train staff on the correct use of RT/LT, 59, and 76 modifiers. Use prompts within your EMR system to support accuracy.
G. Create a Compliance Checklist
A checklist helps your team stay consistent. It should include:
- Documentation accuracy
- Code verification
- Modifier checks
- Claims submission timeline
- Payer-specific requirements
Consistency reduces errors and speeds up payment.
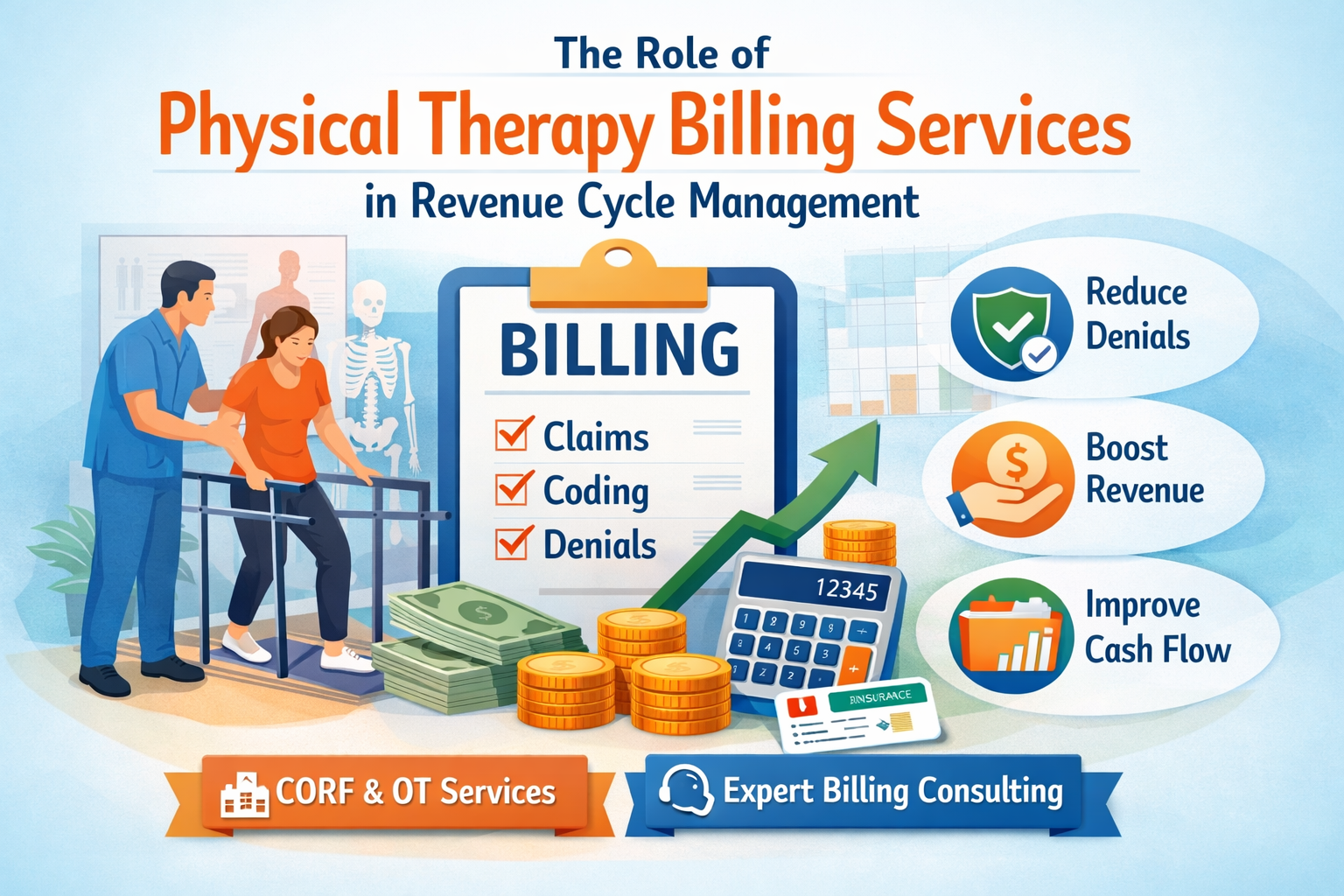
VI. How Outsourcing Respiratory Therapy Billing Can Reduce Errors
Some healthcare practices choose outsourcing when billing becomes too overwhelming. This decision can make daily operations easier and more efficient.
A. When to Consider Outsourcing
Consider outsourcing if:
- Denial rates are rising
- Staff is overwhelmed
- Claims take too long to process
- You’re expanding services
Outsourcing may also help if you’re already using services like OT Billing Services or Physical Therapy Billing Services and want everything under one vendor.
B. Benefits of Outsourcing
Outsourcing brings several advantages:
- Access to certified billing specialist
- Faster claim submissions
- Better documentation review
- Reduced administrative workload
- Improved denial management
Some providers also use outsourced billing for specialized areas such as Corf Services, which require high accuracy and adherence to Medicare regulations. This helps reduce compliance risks and protects reimbursement.
VII. Real Examples of Billing Error Scenarios
To make this more relatable, let’s walk through real-life scenarios you might encounter in a therapy practice.
Case Study 1: Incorrect Modifier Leads to Denial
A therapist provided repeated nebulizer treatments on the same day. The billing team forgot to add modifier 76. The claim was denied. Once the modifier was added, the claim was approved.
Case Study 2: Missing Documentation Causes Underpayment
A clinic billed for pulmonary rehab but didn’t include time logs. The payer adjusted the payment down because the service wasn’t fully documented. After updating the documentation process, future claims were fully paid.
Case Study 3: Duplicate Billing Flagged During Audit
Two staff members billed the same patient for oxygen therapy on the same date. An insurance audit flagged the duplicate. The practice had to refund the payment and update their workflow to prevent repeated submissions.
VIII. Conclusion
Billing mistakes happen, but they don’t have to disrupt your entire workflow. When you understand the most common errors, you’re already on the path toward preventing them. The key is staying proactive. Update coding knowledge. Strengthen documentation. Use technology where it helps. And don’t hesitate to get expert support when the workload becomes too heavy.
With the right systems and consistent training, your team can reduce denials, speed up claim approvals, and protect your practice’s financial health. Whether you’re handling respiratory therapy billing in-house or coordinating with partners who offer solutions such as Tools and Software to Simplify Medicare Billing, clear processes lead to better outcomes and fewer problems.
Remember, billing doesn’t need to feel overwhelming. Small improvements add up. And each time you prevent an error, you make your entire workflow smoother.