I. Introduction
Pelvic pain is something many patients struggle with, yet it often goes undiscussed. You probably see this in your clinic too. Some patients mention pelvic pain quietly and almost as an afterthought. Others only bring it up when the pain becomes overwhelming. Pelvic pain can affect anyone, but it is especially common among women.
In practice, we see pelvic pain connected to muscular problems, gynecologic issues, urinary symptoms, bowel problems, and even stress. Because the causes vary, the work of diagnosing, documenting, and coding pelvic pain becomes more important and sometimes more confusing for clinicians.
That’s where accurate ICD-10 coding comes in. Getting the right pelvic pain ICD-10 code is more than just a billing requirement. It helps you establish medical necessity, prove the patient needs care, and support continuity of treatment across providers. Good documentation also protects you from risk and improves communication between referring doctors, pelvic floor therapists, and other members of the care team.
In this guide, we’ll walk together through the basics of pelvic pain, the ICD-10 codes you’ll use, what to document, and how to plan care. Think of this as a friendly walk-through — like something you’d explain to a colleague over coffee. You’ll also see a few real-life examples, because those always make clinical topics easier to understand.
II. Understanding Pelvic Pain: Clinical Overview
A. What Qualifies as Pelvic Pain?
Pelvic pain is usually described as discomfort, pressure, or sharp pain in the lower abdomen or pelvis. It may come and go, or it may stick around for months.
You’ll often hear two terms:
- Acute pelvic pain — sudden and lasting a short time.
- Chronic pelvic pain — lasting longer than 6 months.
Chronic pelvic pain is particularly tricky because it doesn’t always have a single clear cause. Some patients bounce between providers for years before finding relief.
Common Causes
Pelvic pain can stem from several systems in the body:
- Musculoskeletal — tight muscles, pelvic floor dysfunction, low back problems
- Gynecologic — endometriosis, ovarian cysts, dyspareunia
- Urologic — urinary urgency, bladder pain, recurrent UTIs
- Gastrointestinal — constipation, IBS
- Neurologic — nerve irritation, pudendal neuralgia
Sometimes, despite a full workup, we still don’t find a clear cause. That’s when pelvic pain becomes a diagnosis of exclusion meaning other dangerous conditions were ruled out first.
B. Symptoms & Clinical Presentation
Patients may report:
- Localized pelvic aching
- Shooting or radiating pain
- Muscle tightness
- Pain with sitting
- Pain during intimacy
- Difficulty with bowel movements
- Pressure or heaviness
You’ll often notice a mix of symptoms. Pelvic pain rarely exists on its own. You might hear about urinary urgency, constipation, low back pain, or even pelvic floor tightness.
C. When to Classify Pelvic Pain under ICD-10
You use pelvic pain ICD-10 coding when:
- No clear cause is found, or
- The documentation supports symptom-based coding, or
- Pelvic pain is secondary to a more specific condition
If you identify a more specific root cause (like endometriosis or IBS), you should code that too.
III. ICD-10 Codes for Pelvic Pain
A. Primary Pelvic Pain ICD-10 Code
Let’s start with the code you’ll use most often.
• R10.2 – Pelvic and perineal pain
This is your go-to symptom code when pelvic pain is present but you don’t yet have a confirmed diagnosis. You’ll use it when:
- The patient reports pelvic or perineal pain
- You’ve ruled out emergencies
- You’re working through a care plan
- A specialist referral is pending
R10.2 is simple, but it requires strong documentation. A vague chart note won’t cut it.
B. Related ICD-10 Codes
Sometimes pelvic pain is linked to an underlying condition. Here are common codes based on systems.
GYNECOLOGIC CAUSES
- N94.10 – Unspecified dyspareunia
- N94.2 – Vaginismus
- N94.4 – Primary dysmenorrhea
- N94.5 – Secondary dysmenorrhea
- N80.xx – Endometriosis (multiple codes)
UROLOGIC CAUSES
- R39.15 – Urinary urgency
- N30.xx – Cystitis
- N35.xx – Urethral stricture
GASTROINTESTINAL CAUSES
- K59.00 – Constipation, unspecified
- K58.xx – Irritable bowel syndrome
MUSCULOSKELETAL / PELVIC FLOOR
- M62.830 – Muscle spasm of back
- M62.89 – Other muscle disorders
- M54.5 – Low back pain
- M53.3 – Sacrococcygeal disorders
C. Red-flag diagnosis exclusions
Never assign R10.2 until you’ve ruled out emergencies like:
- Appendicitis
- Ectopic pregnancy
- Ovarian torsion
- Pelvic inflammatory disease
- Acute infections
These require urgent or emergency care.
IV. Clinical Documentation Requirements
Let’s talk about the kind of notes that actually support the ICD-10 code you chose. Great documentation protects you and helps the patient get the right care.
A. Key documentation elements
Include:
- Pain location — where exactly in the pelvis?
- Pain quality — sharp, dull, burning?
- Duration — acute or chronic?
- Functional limits — sitting, walking, intimacy
- Symptoms — urinary, bowel, reproductive
- Triggers — exercise, lifting, menstrual cycle
- Relief — stretching, warm baths, medication
- Objective findings — pelvic exam, posture, muscle tightness
Short sentences help. Long paragraphs make it harder for the reviewer.
B. Pelvic floor–specific documentation
Pelvic floor therapists often note:
- Hypertonicity (tightness)
- Weakness
- Muscle tenderness
- Trigger points
- Internal or external exam findings
You want your note to paint a clear picture. Imagine someone else reading your note and understanding exactly what happened.
C. Linking symptoms to function
This is vital for medical necessity.
Instead of writing:
“Patient has pelvic pain.”
Try:
“Pelvic pain limits sitting longer than 20 minutes and makes intimacy painful.”
Simple, clear, and functional.
D. Documentation phrases that help ICD-10 accuracy
You can use phrases like:
- “Pain affects functional mobility…”
- “Pelvic floor hypertonicity is present…”
- “Pain limits sexual function and ADLs…”
These statements also support therapy coverage, especially when dealing with insurance reviewers.
V. Care Planning for Pelvic Pain
A care plan gives structure and direction. It tells the patient what to expect and helps you track progress.
A. Establishing goals
Common goals include:
- Lower pain
- Improve pelvic floor coordination
- Improve bladder or bowel habits
- Improve intimacy
- Increase sitting or lifting tolerance
- Reduce stress and tension in the muscles
B. Evidence-based interventions
Here’s what typically works:
Pelvic Floor Therapy
- Manual therapy
Gentle releases and mobilization. - Biofeedback
Helps the patient learn how to relax or activate muscles. - Soft tissue mobilization
Internal or external work. - Relaxation training
Often includes breathing strategies. - Coordination training
Teaching the patient to activate muscles at the right time. - Trigger point release
Helps reduce tight knots in the pelvic floor.
If your clinic uses ot billing units, you might see how pelvic health overlaps with other therapy services. The same is true in PT clinics offering physical therapy billing services where pelvic pain treatment also blends into musculoskeletal care.
Medical Interventions
- NSAIDs
- Hormonal treatment
- Antibiotics for infections
- Thermal therapy
- Chronic pain referral
Behavioral Approaches
- Relaxation
- Stress reduction
- Diaphragmatic breathing
- Posture changes
- Lifestyle improvements
C. When to refer
Refer when pelvic pain involves:
- Severe pain
- Infection signs
- Gynecologic emergencies
- Possible malignancy
D. Care plan documentation language
You can write:
- “Patient will attend 1–2 sessions per week for 8–12 weeks.”
- “We will focus on pelvic floor relaxation and coordination.”
- “Progress will be monitored with function-based tests.”
When clinics expand services, they sometimes add corf services, which also address chronic pelvic conditions. Some teams even explore CORF vs. Home Health models to decide which setting fits patient needs better.
VI. Billing & Coding Considerations
Billing can feel overwhelming, but once you understand the essentials, it becomes manageable.
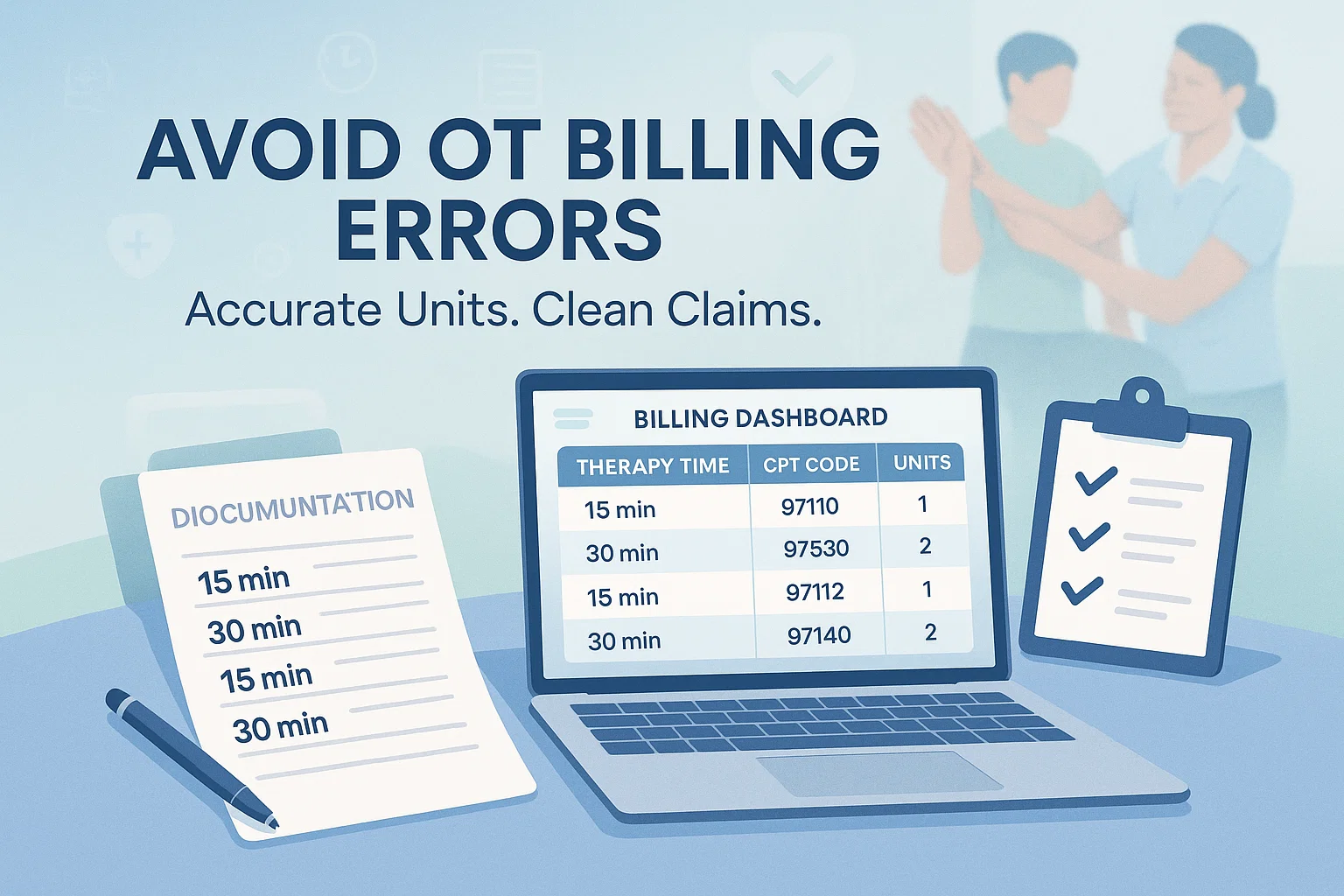
A. Pairing ICD-10 with CPT Codes
Common therapy CPT codes include:
- 97110 – Therapeutic exercise
- 97112 – Neuromuscular re-ed
- 97140 – Manual therapy
- 97530 – Therapeutic activities
- 97014/97032 – Modalities
If your clinic works across multiple service lines, things like corf services may overlap. Some providers also look at CORF vs. Home Health options, especially when deciding where pelvic pain therapy fits best.
B. Avoiding common billing mistakes
Watch out for:
- Using R10.2 without good documentation
- Ignoring a more specific diagnosis
- Missing functional impairment details
- Forgetting to link interventions to medical necessity
Clinics that track ot billing units or rely on physical therapy billing services already understand how small documentation gaps can lead to claim denials.
C. Payer requirements
Watch for:
- Medicare rules
- Commercial payer policies
- Prior authorization limits
And stay aware of The Future of Physical Therapy Billing, because billing trends continue to shift. In fact, awareness of these trends helps both pelvic health therapists and general outpatient clinics adapt care plans efficiently. Many training programs now talk about The Future of Physical Therapy Billing, especially as new CPT bundles and digital health codes emerge.
VII. Case Examples
Let’s walk through a few examples to make the process clearer. Stories help us apply guidelines in real life.
Case 1: Muscular Pelvic Pain
A 32-year-old reports tight, stabbing pelvic pain. She struggles to sit longer than 15 minutes. The exam shows pelvic floor tightness, tenderness, and poor relaxation.
ICD-10: R10.2 + M62.89
Documentation Example:
“Pelvic pain increases with sitting. Pelvic floor hypertonicity and tenderness on exam.”
Case 2: Dyspareunia
A patient reports deep pelvic pain during intimacy.
Exam shows tenderness around the vaginal opening and increased muscle tone.
ICD-10: N94.10 or N94.2 depending on findings.
Case 3: Chronic Pelvic Pain of Unknown Cause
A patient has seen multiple providers and no definitive cause has been found. Symptoms include constant pelvic aching and difficulty lifting.
ICD-10: R10.2
Justification:
Document function limits clearly, such as difficulty with walking or lifting.
VIII. Patient Education & Self-Management
Teaching patients how to help themselves is part of the plan.
Home Exercises
- Gentle stretching
- Pelvic floor relaxation
- Bridges and core work when appropriate
Breathing & Relaxation
Slow belly breathing reduces tension.
Heat/Ice
Heat helps muscle tension. Ice can help with inflammation.
Lifestyle Adjustments
- Hydration
- Avoiding bladder irritants
- Improving posture
- Reducing long sitting sessions
Bladder/Bowel Habits
Regular habits lower pelvic stress.
When to Seek Urgent Care
Explain red flags clearly.
IX. Conclusion
Pelvic pain is common, but with the right ICD-10 coding, strong documentation, and a thoughtful care plan, you can guide patients toward relief.
Good notes protect you. Accurate codes protect reimbursement. Clear plans guide treatment.
As the healthcare world evolves from outpatient clinics to discussions around CORF vs. Home Health, and even shifts connected to The Future of Physical Therapy Billing staying informed helps you deliver the highest level of care.
If your team already handles things like ot billing units or partners with physical therapy billing services, then you know how much good documentation matters. Strong coding and clear care planning isn’t just about billing. It’s about making sure your patient gets exactly what they need.
Pelvic pain is personal and often frightening for the people who experience it. The way you document, code, and plan care can make their journey smoother and help them feel supported every step of the way.