I. Introduction
If you’ve ever worked in occupational therapy, you know that billing can feel like a maze. Between coding, time tracking, and insurance rules, it’s easy to get lost. That’s why understanding OT billing units is crucial. Whether you’re an OT practitioner, a billing specialist, or just curious, this guide will make the whole process clear.
Accurate billing isn’t just about getting paid. It affects compliance, patient records, and reimbursement. Even a small mistake in units or codes can lead to denied claims, frustrated patients, or unnecessary audits.
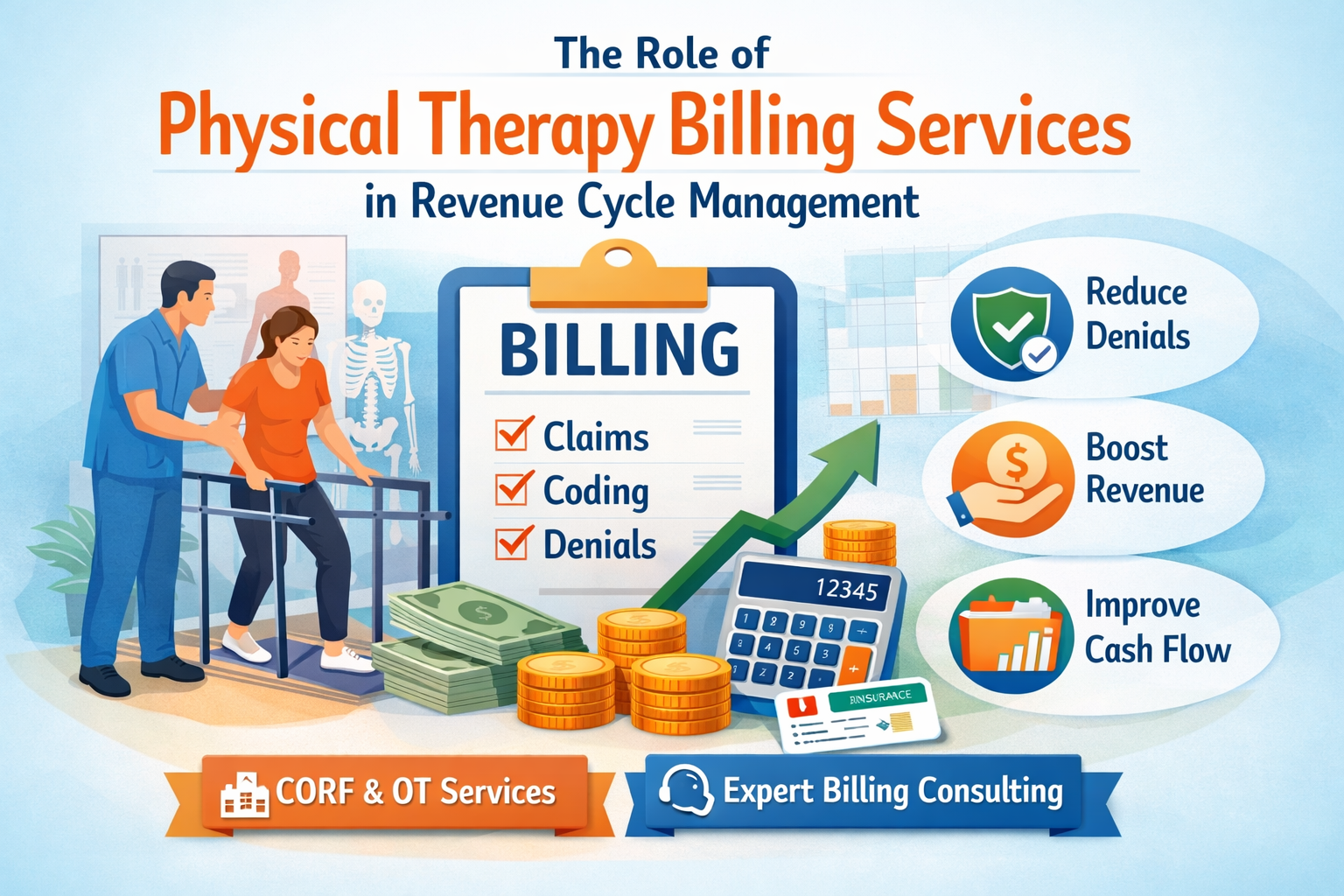
By the end of this guide, you’ll know exactly what OT billing units are, how to calculate them, common pitfalls to avoid, and some handy tips from the field. Think of this as a friendly conversation over coffee about Occupational Therapy Billing Services, Physical Therapy Billing Services, and how to navigate the sometimes tricky world of CORF Services in 2025.
II. What Are OT Billing Units?
Let’s start with the basics. OT billing units represent the time or service provided during an occupational therapy session. Insurance companies use these units to determine reimbursement.
Here’s a simple analogy: if your therapy session is like a pizza, the billing units are the slices. You get paid per slice, so you need to count them correctly.
There are two main types of units:
- Time-based units – These are measured in minutes, usually in 15-minute increments. For example, a 30-minute session is typically billed as 2 units.
- Service-based units – Some codes are billed as a whole unit regardless of session length, such as a specific evaluation or consultation.
Units tie directly to OT billing codes, which help insurers understand exactly what service was provided. Without them, you can’t submit accurate claims.
III. Common OT Billing Terminology
Before we dive deeper, let’s get familiar with some common terms:
- CPT Codes: These codes specify the type of OT service provided. For example, 97165 is often used for an initial evaluation.
- HCPCS Codes: These are similar to CPT codes but cover different services or supplies, like durable medical equipment.
- Timed Units: These are calculated based on how long you spend with a patient, usually in 15-minute increments.
- Treatment vs. Evaluation Codes: Evaluations are billed differently from treatments. For example, an initial assessment might be billed as 1 unit regardless of time, while therapy sessions are time-based.
- Modifiers: Sometimes you need a little extra detail for insurance. Modifiers show if a session was split, repeated, or had another special circumstance.
Understanding these terms will make calculating and documenting units much easier.
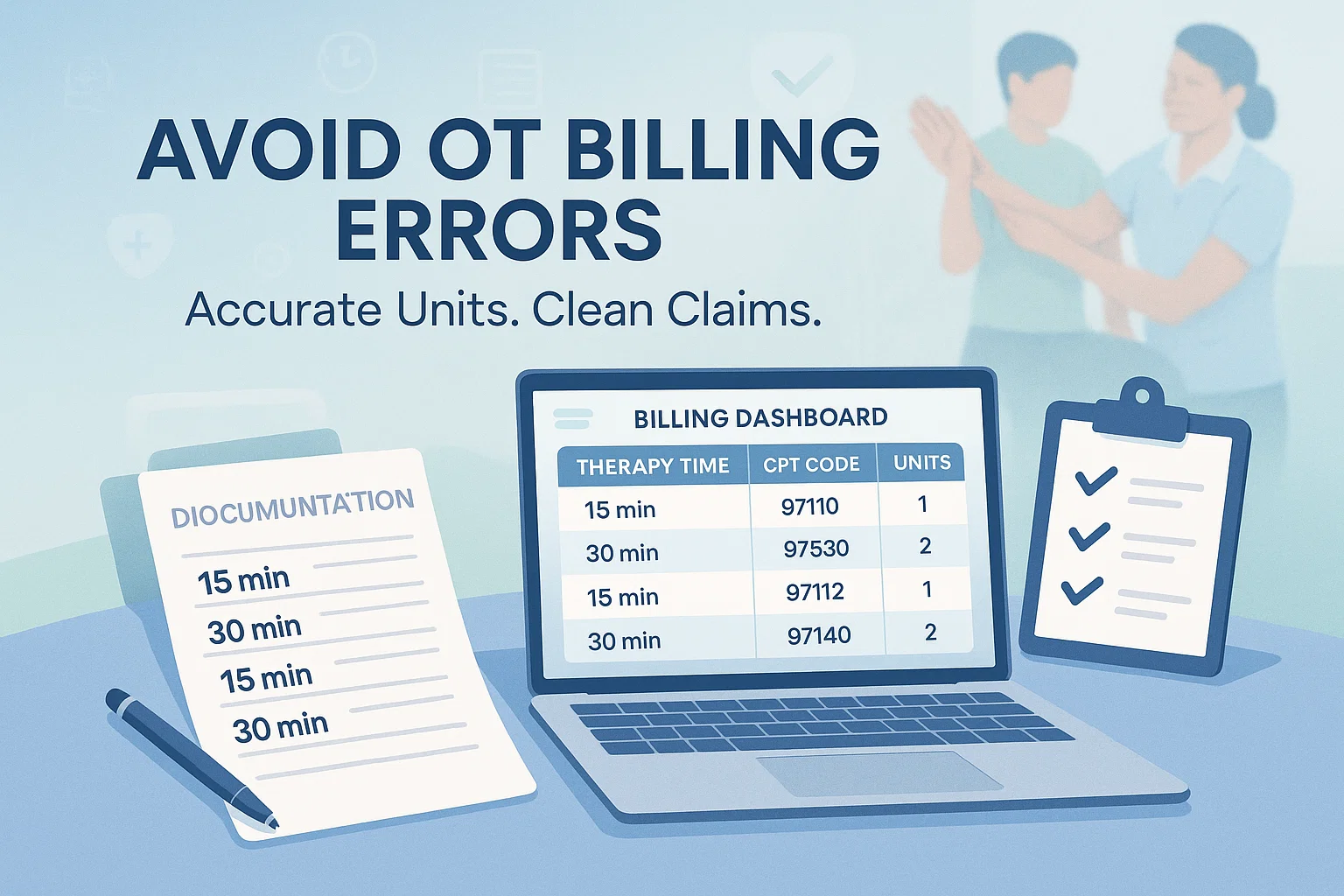
IV. How OT Billing Units Are Calculated
Calculating units may seem tricky, but once you break it down, it’s pretty straightforward. Here’s a step-by-step approach:
- Determine Session Length: Note exactly how long you spent with the patient.
- Identify the Correct CPT/HCPCS Code: Each service has its own code.
- Calculate Units: For timed codes, divide total session minutes by 15 to get units.
Examples:
- 30-minute session → 2 units (15 minutes = 1 unit)
- 45-minute session → 3 units
- 50-minute session → 3 units (partial units are typically rounded according to payer rules)
A tip from experience: always check insurance guidelines. Some payers round differently, and knowing this can save headaches later.
V. OT Billing Units by Setting
Billing units can vary depending on where you provide therapy:
- Inpatient Rehab: Usually shorter sessions with strict unit tracking. Frequent evaluations may require separate codes.
- Outpatient Clinics: Sessions are typically 30-60 minutes. You might combine OT billing codes for different services provided in one session.
- Home Health: Travel time can sometimes affect billing, and combined therapy sessions may require special attention.
- School-Based OT: These sessions often have unique considerations, especially if therapy is integrated into the classroom schedule.
Understanding the setting helps you bill accurately and avoid denied claims.
VI. Documentation and Compliance
Documentation is your best friend when it comes to billing. Good notes prove the units you billed are accurate. Include:
- Time spent on each intervention
- Patient goals and progress
- CPT code justification
This isn’t just for insurance. Detailed notes also help you track patient progress and communicate effectively with other providers. If you’re handling CORF Services, this step is especially critical for audits and compliance in 2025.
Read more on our Medium blog: The Essential OT Billing Units Handbook: Tips, Tricks, and Best Practices.
VII. Common Mistakes in OT Billing Units
Even experienced OTs make mistakes. Watch out for:
- Overbilling or underbilling units
- Confusing timed vs. untimed codes
- Missing documentation
- Forgetting necessary modifiers
Mistakes can be costly. Not only can claims be denied, but repeated errors may trigger audits.
VIII. Tips and Best Practices
Here are some practical tips:
- Keep detailed time logs – don’t rely on memory.
- Use billing software or templates for accuracy.
- Regularly review payer policies to stay compliant.
- Communicate with colleagues or billing specialists when unsure.
For clinics handling both OT and Physical Therapy Billing Services, consistent procedures across disciplines can save time and prevent errors.
IX. Resources and Tools
You don’t have to figure this out alone. Here are some helpful resources:
- Official CPT and HCPCS guides – essential for correct coding.
- Recommended OT billing software – tools like WebPT, Kareo, or TherapyNotes.
- Professional associations – AOTA (American Occupational Therapy Association) and CMS provide guidelines, webinars, and support.
Keeping these resources handy ensures you stay compliant and maximize reimbursement for Occupational Therapy Billing Services.
X. Conclusion
Accurate billing is vital for every OT professional. Understanding OT billing units ensures compliance, proper documentation, and fair reimbursement. Whether you’re handling CORF Services, running an outpatient clinic, or managing Physical Therapy Billing Services, knowing how to calculate units properly makes your job easier.
Take some time today to review your current billing practices. Are your units accurate? Are you using the right codes and modifiers? Implementing these strategies can save time, prevent denied claims, and keep your patients and insurance providers happy.
Remember: proper billing isn’t just a task. It’s a skill—and one that can make your professional life much smoother.
FAQs About OT Billing Units
Q: Can units be combined in a single session?
A: Sometimes, yes. If you provide multiple distinct services, each with its own CPT code, you can bill separately—but check payer rules.
Q: How do insurance audits affect billing units?
A: Audits review documentation against billed units. Accurate notes and correct codes reduce risk of claim denials.
Q: Are there differences in billing units by state?
A: Absolutely. Some states have unique rules for CORF Services in 2025 or Medicaid billing. Always review local guidelines.