Sarah, a stroke patient, required six weeks of occupational therapy after a brain stroke to regain independence to execute daily tasks like eating, cooking, and dressing. Sarah diligently attended her therapy sessions, making good progress in her recovery. However, she faces recurring issues with her medical bills. Inaccurate billing units for occupational therapy and clinical records, such as calculation errors, vague terms or language, delayed entry, incorrect coding, and documentation errors, appear to be time-consuming and challenging for both the therapist and patients. People spend hours communicating with the billing department supervisor or insurance company officials through emails or phone calls for rectification, which leads to frustration and anxiety.
Ongoing billing turmoil, such as a lack of transparency in billing units, inconsistent medical records, allows therapists to forget significant details or the exact amount of time spent on a therapy task. Inaccuracies in billing make it difficult for therapists to focus on therapy, especially when transitioning quickly between sessions and therapy exercises. Over-documenting, chasing down missing entries, and reconciling hours further make it hard for office managers to track client progress or justify their treatment procedures to insurers. Lack of an audit trail further causes inconvenience to clinical therapists, such as compliance risks and billing discrepancies.
The blog provides an ultimate guide to OT billing units to help therapists know about OT billing and CPT codes, develop the ability to calculate, and optimize their OT billing units. The medical experts learn practical time-tracking tips that improve accuracy and reduce denials. They get knowledge about using the 8-minute rule for time-based services. The therapists are required to complete patient documentation in real time and correctly code evaluations. Moreover, using technology such as Electronic Health Record (EHR) systems helps in streamlining therapy practices, such as providing accurate documentation and sending automated reminders for coding updates. The other techniques help in conducting regular audits, allowing health professionals to maintain compliance standards and boost the clinic’s revenue and profit.
Understanding OT Billing Units
As defined by the American Occupational Therapy Association, occupational therapy is considered a significant part of clinical practice that helps provide a groundwork for accurate documentation and billing services. OT billing units are a standardized method of measuring the amount of service an occupational therapist provides to a client. A precise billing method with detailed documentation of the therapy service provided demonstrates that the treatment is clinically appropriate and effective. Moreover, accurate billing units help payers receive financial reimbursement through Medicare/Medicaid and other insurance companies.
Occupational therapy billing services include two types of codes. Timed and untimed codes.
Timed Codes
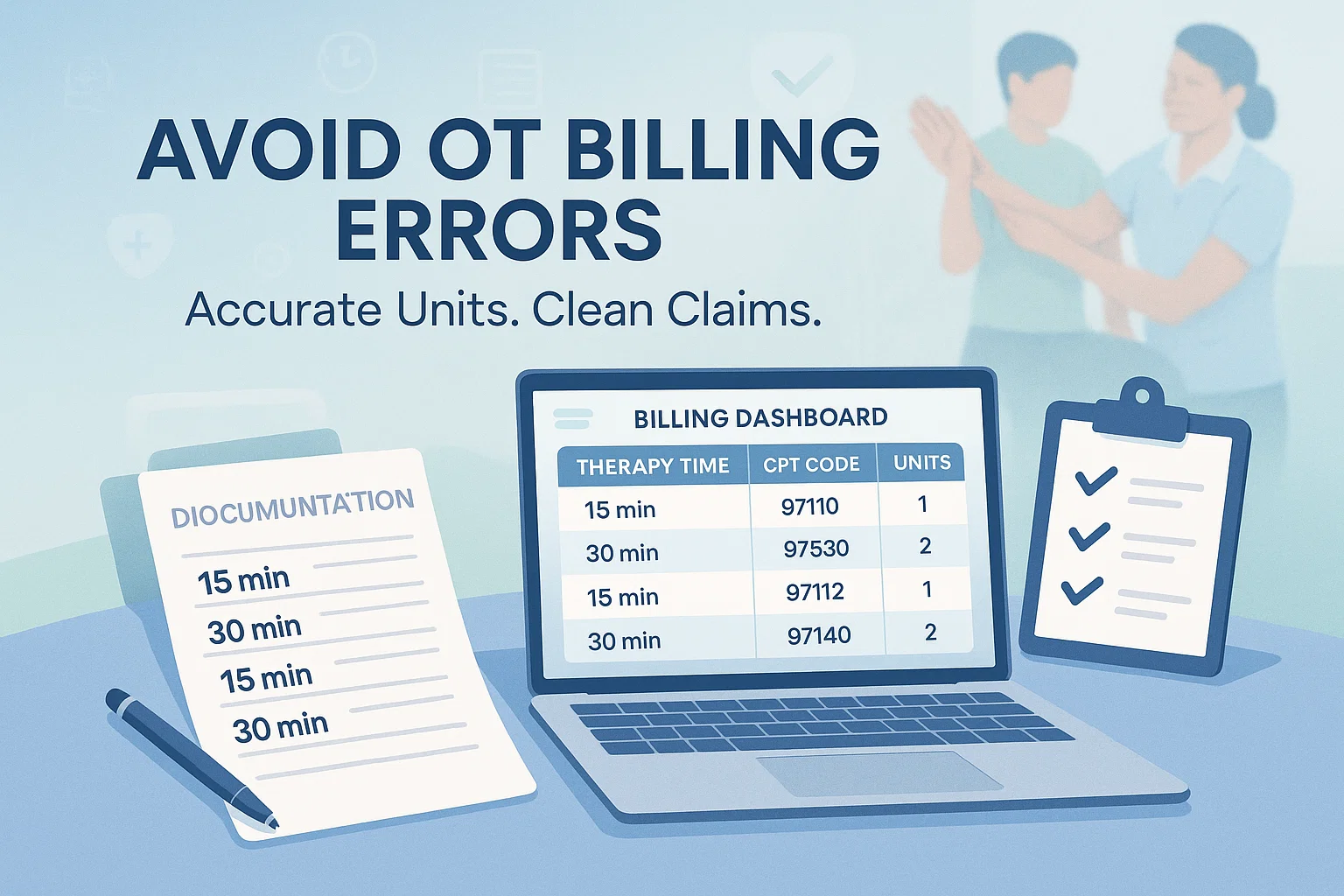
The therapists use these codes for services that involve direct, one-on-one contact with the patient. Applying the 8-minute rule, these services are charged based on the duration of the service. Billing units are timed services, dividing time into 15-minute blocks. For instance,
1 Unit: 8-22 minutes, 2 Units: 23-37 minutes, 3 Units: 38-52 minutes,4 Units: 53-67 minutes, and so forth, in 15-minute increments.
Untimed Codes
These service-based codes allow therapists to bill one unit per session for evaluations regardless of the time spent to complete the service. It includes evaluation codes for low complexity, allowing the therapist to know the brief medical history of the patient in a 30-minute duration.
The CPT code for moderate complexity includes gathering an extended medical history in 45 minutes. Conducting high complexity OT therapy services comprises 60 minutes, detailed medical history of the patient. The other CPT code is used for re-evaluation, such as changing the plan of care based on the patient’s progress.
The most commonly used CPT codes are applied for therapeutic activities for functional improvement, self-care activities, and learning ADL/IADL skills. Therapeutic exercise codes strengthen the brain-body connection, develop endurance, and flexibility. The therapist uses CPT codes for community and work reintegration. The trained therapist guides a small group of patients to engage in group therapy exercises. The patients learn healthier ways of skill-building and improving interpersonal relationships.
Common Time-Tracking Challenges in OT
Inconsistent Start/Stop Recording
Administrative burden causes fatigue, potentially leading to burnout among therapists. Regulatory strain leads to inefficiency in documentation, such as inconsistent start/stop recording in occupational therapy. The absence of clear, practical, and standardized guidelines for OT billing units results in disorganized documentation and leads to reporting errors. Thus, fragmented and patchy recording in occupational therapy also makes it difficult for therapists to make an insurance claim. In most cases, document discrepancies lead to insurance rejections as insurance companies depend on accurate and consistent information to assess risk and coverage.
Multitasking During Sessions
Multitasking issues that most occupational therapists encounter are co-treatments, interruptions, and concurrent tasks. An intense clinical setting, along with unsystematic data management, brings chaos and potentially interrupts the therapeutic sessions. It makes it difficult for therapists to deal with one patient at a time and manage their documentation, progress reporting, and plan organizing flexible therapy sessions. Therefore, switching back and forth between multiple patients disturbs their scheduling and also affects their work performance and service delivery rate.
Manual vs. Digital Tracking Errors
Manual tracking in physical therapy billing services is vulnerable to common errors, such as inaccurate coding. The manual process of writing complex codes, such as CPT codes and modifiers, may cause errors in coding. It includes creating inconsistent and jumbled codes that lack clarity. Obscure codes with logic errors, hidden messages, and concurrency issues. Manual data entry causes errors in recording patient details, insurance information, service dates, and inadequate and missing documentation. Incompetency in manual documentation also causes miscalculation, such as underbilling or overbilling. Consequently, the payers fail to get insufficient progress reports and follow-up details. Furthermore, improper authorization leads to insurance coverage denial.
As compared to digital tracking systems, having automation features helps occupational therapists with real-time automated eligibility checks. The billing tools streamline the documentation procedure, diminishing data entry and coding errors. Furthermore, digital tracking assists patients with easier tracking of claims, a faster payment process, and leads to speedy insurance verification in medical billing.
Misalignment with CPT Code Requirements
Discrepancies with CPT code requirements include loopholes in the patient’s documentation and improperly calculated time-based CPT codes, such as therapeutic exercise and manual therapy sessions. Misalignment makes it difficult for the therapy analyst to translate codes to units, and they make wrong code selections. Different therapy procedures are undertaken by using a single CPT code or multiple codes for the same procedure indicates inefficiency in handling CPT codes.
Misalignment in coding or missing information results in automatic insurance claim rejection, payment delays, and other financial and legal penalties.
Boost OT Billing Accuracy with Better Tracking
Tip 1: Always Document Start and Stop Times Immediately
To reduce documentation burden and improve the documentation workflow, occupational therapy billing services use practice management software (PMS) or Electronic Health Record (EHR) systems that syndicate billing with clinical workflows. The software helps therapists with real-time logging and consistent monitoring of the start and end times of therapy exercises. The tools also provide accurate scheduling, the patient’s progress report, the therapist’s signature, and the therapy session date and the type of therapy provided. The electronic Medical Record (EMR) systems ensure transparency in OT billing units, providing an accurate and smooth billing procedure.
Tip 2: Break Sessions into Billable and Non-Billable Segments
An ultimate guide to OT billing units allows occupational therapists to use a billing software that is synced with the automated time tracker. The tools allow professional experts to quickly monitor billable hours tasks that include conducting client meetings, spending time on project work such as writing code, creating flexible therapy plans, and conducting client research. The other billable hours comprise administrative tasks that include communicating with clients through emails or via calls to provide therapy session updates and CPT codes to avail specific therapy services. Moreover, tracking billable hours includes registering the mandatory breaks during work and ensuring safety and fatigue management.
Non-billable tasks comprise internal administrative tasks such as sending internal emails to teams for scheduling in-house meetings, and improving networking. Setting up the latest equipment, such as practice management software and AI-powered clinical support and documentation tools, supports occupational therapy billing services to manage appointments, standardize billing and insurance, determine reimbursement, and ensure an accurate payment system for patients.
Moreover, AI documentation tools also streamline the payroll system. Client engagement software keeps patients informed about performing mindfulness exercises between sessions. The therapist also uses therapy tools such as Talkcast, which improve interaction between therapists and patients. Furthermore, personalized mini-podcasts by therapists reinforce patient education to enhance their understanding of diagnosis and treatment, the type of therapy required, help patients know the recovery progress, and demonstrate the reasons for continued therapy services.
Tip 3: Follow the 8-Minute Rule Correctly
The latest Medicare rules for therapy billing in 2025 enable therapists to utilize the Medicare Part B 8-Minute Rule for providing outpatient therapy services such as physical, occupational, and speech therapy, ensuring precise reimbursement for time-based CPT codes. Therapists engage in a minimum of 8 minutes of direct, face-to-face interaction with the patient. Following the initial 8 minutes, each additional unit is accrued in 15-minute intervals. For instance, 8–22 minutes equals 1 unit, 23–37 minutes count as 2 units, 38–52 minutes amount to 3 units, and so on. To guarantee accurate documentation of therapy time, therapists employ time-tracking software that meticulously logs session notes, including the exact starting and ending times for each timed service, the variety of therapeutic exercises administered, and the patient’s reaction to the treatment.
Tip 4: Use Digital Time-Tracking Tools or EMR Timers
Maintaining precise and legal documentation in pulmonary therapy services, such as billing and reimbursement, legal compliance, quality assurance, and tracking productivity, allows therapists to employ digital time-tracking tools and EMR (Electronic Medical Record) timers. An efficient EMR system with a built-in timer is synchronized within the patient’s chart. As therapy begins, the therapist starts the timer and stops it when the session ends. The tools track time spent on pulmonary therapy exercises such as energy conservation techniques training, pursed-lip breathing, and diaphragmatic breathing, and tolerance and endurance training. The dedicated time-tracking software automatically records the activity duration, therapeutic exercise, CPT code integration, and accurate unit calculation that leads to an efficient billing and reimbursement process.
Tip 5: Track Multi-Modal Interventions Separately
The occupational therapy billing service tracks different multi-modal interventions involving patients’ documentation and different forms of occupational therapy activities.
The billing service for occupational therapy monitors various multi-modal interventions while managing patient documentation and different occupational therapy activities. It involves recording the precise duration spent on each modality during a session. For example, a 10-minute preparatory session helps clients understand various occupational therapy techniques, including heat, cold, electrical stimulation, orthotics, and prosthetics therapy, as well as using technology for therapeutic exercises. A 15-minute self-care training enhances manual and sensory motor skills necessary for independently performing household tasks. By effectively employing modern tracking methods and tools, therapists can accurately assess motor and cognitive-perceptual skills and track patient progress.
To track and bill for multimodal interventions, therapists utilize specific CPT codes that correspond to the therapeutic services rendered. Therefore, occupational therapists implement standardized assessments and structured documentation techniques to manage the multimodal treatment plan, which aims to address clients’ changing requirements, such as self-care/home management and the development of cognitive skills
It includes recording the specific amount of time spent on each distinct modality during a session. For instance, 10 minutes of a preparatory session that helps clients know about various occupational therapy techniques encompassing heat, cold, and electrical stimulation, orthotics, and prosthetics therapy sessions, and using technical tools for therapeutic exercise.15 minutes of self-care training improves manual and sensory motor skills to perform dressing, eating, and other household tasks independently. Utilizing the modern tracking methods and tools effectively assesses motor and cognitive-perceptual skills, tracks therapy goals and outcomes over time, and provides accurate and comprehensive subjective data on patient progress.
For tracking and billing multimodal interventions, the therapist uses specific CPT codes that are based on therapeutic services provided. Thus, occupational therapists use standardized assessments and structured documentation methods to regulate the multimodal treatment plan, aiming to meet clients’ evolving needs, including self-care/home management and building cognitive skills.
Tip 6: Create a Standardized Workflow or Templates
An ultimate guide to OT billing units helps occupational therapists establish a standardized workflow for effective documentation. This means that the documentation analyst adheres to three essential steps of the OT process: evaluation, intervention, and outcomes. In the evaluation phase, the therapist develops an occupational profile by gathering pertinent patient information, including daily routines, work, play, leisure activities, and physical/cognitive abilities. The intervention step enables therapists to create a personalized treatment plan aimed at enhancing functional and cognitive skills. The outcomes also aid healthcare professionals in tracking the patient’s progress and supporting a comprehensive therapy plan. The treatment plan is formulated by a multidisciplinary team that aims to provide personalized, consistent care for patients.
Tip 7: Audit Your Time Logs Weekly
Another strategy that helps bring accuracy in OT billing is to audit time logs weekly. Physical therapy billing services conduct a structured process to analyze professional goals and improve client outcomes. A weekly audit helps in tracking precise time logs, allowing therapists to record every activity and the time spent on different therapeutic trainings in real-time. Specialized time-tracking software also monitors billable and non-billable work, including breaks and rest periods.
The audit process identifies discrepancies in OT units, such as unit mismatches, patterns of underbilling, or overbilling helps OTs manage time effectively, reduce documentation burden, and enhance overall productivity. Transparent auditing ensures rigorous time tracking and general time management, and correct client billing. To maximize treatment efficacy, therapists adjust therapy plans and prioritize tasks. Moreover, they use specialized billing tools to conduct regular evaluations to optimize treatment plans and boost patient outcomes.
Tip 8: Train Staff on Billing Rules Regularly
Performing regular, ongoing staff training helps enhance occupational therapy practice. It implies that occupational therapy billing services implement a comprehensive training program for OTs and OTAs. Standardized training modules provide knowledge of CPT codes, modifiers, and the 8-minute rule. Therapists, documentation officers, and billing personnel comprehend code usage and evolving billing regulations and payer policies.
To train OT staff on documentation implies that skill-focused therapists know the correct method of documentation that involves knowing about the patient’s diagnosis, treatment goals, and specific therapy services required. Professional training using hands-on sessions elevates skilled services and therapeutic goals. Training OT through mock case scenarios and role-playing documentation helps therapists to develop skills such as clinical reasoning. Therapists analyze complex, simulated patient information in real-time and prioritize interventions. Boosting client-therapist communication allows OTs to discuss the treatment plan with a client and their family in a safe and controlled environment. Moreover, therapists learn to create progress reports and perform proper billing methods. Organizing quarterly or semi-annually training sessions allows therapists to review new Medicare/Medicaid billing regulations, identify new billing trends to enhance treatment plans.
Tip 9: Use Checklists for Complex Cases
To enhance therapeutic outcomes, occupational therapy billing services employ several checklists for precise assessments. Assessment & evaluation phase review healthcare visit, regularize work procedures, monitor co-treatments, and simultaneous therapy. Intervention and case coordination checklists assist therapists in formulating therapeutic objectives, encompassing mental health and cognitive strategies that enhance sleep, energy management, pain coping, and anxiety control. The Intervention and Implementation Checklist monitors client involvement and development, managing intervention throughout different therapeutic environments. Review and Outcome enhance therapists’ abilities and knowledge to handle intricate decision-making processes. Additionally, the teams assess insurer-specific regulations and determine the overall billable time. Consequently, teams recognize the significance of using the checklist to uphold quality and safety standards in occupational therapy.
Tip 10: Avoid Default Time Assumptions
Physical therapy services use customized time tracking for tailored treatment planning and effective, evidence-supported interventions. Real-time tracking helps ensure precise documentation and billing. In addition, the data analyst enhances resource utilization by offering reliable information on services provided, monitoring time allocation among different clients, and overseeing revenue cycles. Consistent time logs demonstrate that the therapist employed the documented time units in providing the necessary therapeutic sessions that support the reimbursement request. Monitoring patients’ progress reflects a therapist’s steady, dependable, and professional approach, which drives positive patient outcomes.
Tip 11: Compliance Considerations
Compliance requires therapists to apply Medicare’s 8-Minute Rule for time-based codes. The therapist keeps detailed records of individual treatment sessions for each billed unit to support claims and avoid denials.
Concerning payer-specific differences, the therapist confirms the unique regulations for unit calculation for each payer. For example, certain payers may determine units according to the overall session duration, like 50 minutes equating to 3 units, while other payers need approximately 50% of the time for a CPT code to be chargeable.
The therapist makes precise documentation of billed units. It involves recording the precise start and finish times for every timed CPT code and verifying that the recorded minutes accurately support the units billed for each code. The therapist synchronizes clinical documentation and billing statements, which allows them to ensure compliance, prevent denials, and facilitate timely reimbursements to clients.
Recap
Understanding precise time tracking is crucial for new occupational therapists. They need to know ethical and legal adherence, precise billing, data-informed treatment planning, and personal professional management to avoid burnout. Novice therapists produce incorrect records that lead to financial repercussions and penalties, and could result in denied insurance claims. As a result, thorough, timely, and precise documentation is essential for ensuring clients receive prompt compensation. To achieve improved treatment results, the therapist creates a comprehensive treatment plan that tracks the patient’s current health condition and utilizes various therapeutic exercises and activities to boost their mental and cognitive abilities. Occupational Therapy services utilize two primary categories of CPT codes. Timed codes require direct, personal interaction with the patient and are charged according to the length of the service provided. The therapist applies the 8-Minute Rule to calculate the units charged for timed services. The second type consists of untimed codes that are charged as one unit, provided that the therapy is administered. Consistent time tracking allows professional therapists to keep precise records. It contains comprehensive session notes that clarify the kind of specialized therapy needed, document the start and end times, or total minutes for each timed service. The analyst records the patient’s reaction to therapy and monitors their progress. To determine healthcare billing compliance, clinical experts ensure that the chosen CPT codes and modifiers correspond with the service provided. Precise coding aids in accurate payments, timely reimbursements, avoids rejections, and ensures compliance with regulations. Transparent and unbiased information additionally aids therapists in modifying treatment plans that align with changing client requirements and enhancing treatment outcomes.
Moreover, continuous internal family systems training and on-site training assist therapists in improving OT therapy skills and contribute to ongoing professional development. To keep up with evolving research in occupational therapy, OT therapists explore additional OT billing resources. It covers detailed materials on coding and billing, available on the AOTA website. Billing manuals, complimentary timesheets, note formats, and therapy-specific resources aid in organizing documentation for every session and noting validated objective patient records. Additionally, employing contemporary therapy and treatment methods, like Electronic Medical Record (EMR) systems, enhances clinical operations and documentation. Therapists utilize Simple Practice and Therapy Notes applications for effective management and precise billing. Printable time-tracking templates enhance treatment effectiveness and guarantee high-quality patient-focused care.